Impact of the COVID-19 pandemic on a healthy and physically active person. Case report and update of the main findings
Impacto de la pandemia por COVID-19 en persona sana y físicamente activa. Reporte de un caso y actualización de los principales hallazgos

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Show authors biography
Introduction. Not all people exposed to COVID-19 develop a severe respiratory disease and the number of young adults without previous pathologies, seriously affected by the virus, is increasing. Many of non-specific symptoms and complications have been evidenced after the recovery.
Objective. To evaluate the repercussions in a healthy and physically active subject who presented serious medical complications and post-COVID-19 complications.
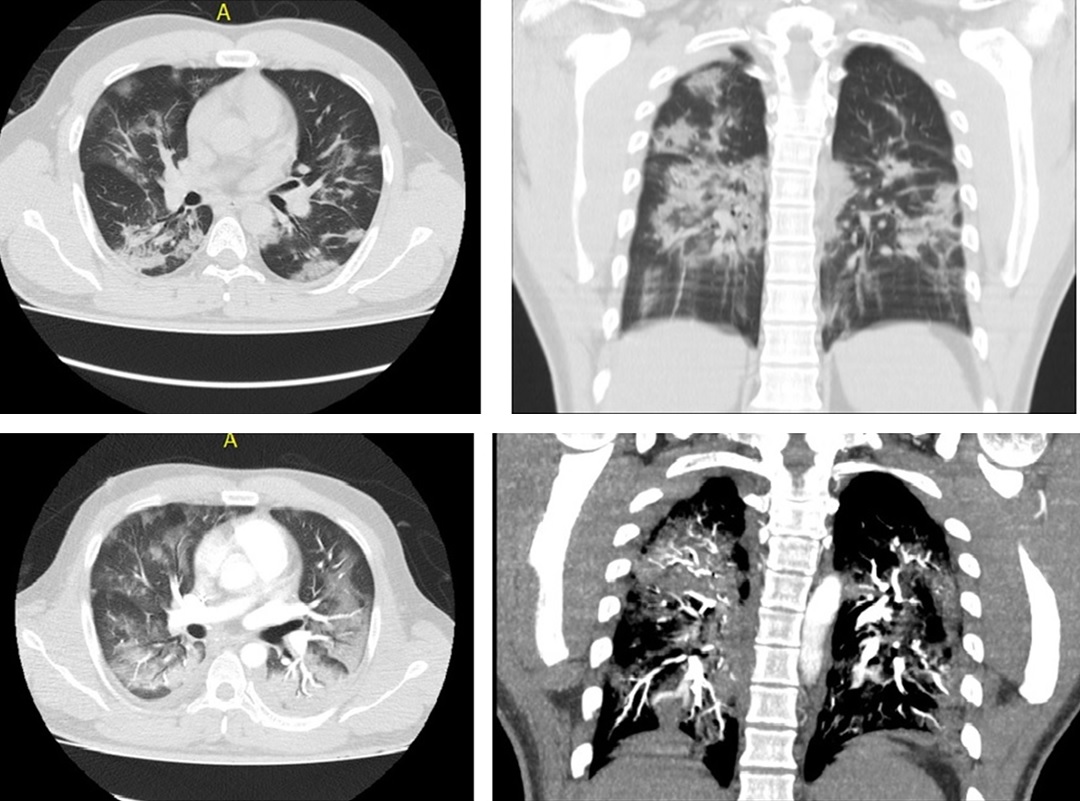
Case report. A 41-year-old man, physically active and without known diseases, in whom SARS-CoV2 infection with a positive PCR test is documented. He required 22 days in the ICU, 17 days in general hospitalization, 57 days of disability and after twelve months there is evident weight and memory loss, difficulty thinking and concentrating, loss of muscle mass, compromised liver function, tiredness and fatigue, muscle pain, sleep problems, changes in mood, and alterations in the taste. According to the current findings, the production of a type of antibody prevents the immune system from having an adequate response against the disease. In addition to this, a new gateway for the virus into the body has been described: the protein neuropilin- 1 (NRP1), as well as the possible decrease in surfactant that allows the flexibility of the lungs. This could provide answers to complications in healthy and physically active people after COVID-19 infection.
Conclusions. Understanding that COVID-19 is a recent disease, there is still a lot of information to collect to understand its behavior in the human body. However, research is providing evidence on why COVID-19 can cause serious medical complications in healthy and physically active people. Understanding that it is a multifactorial situation, more research is necessary with this population in order to carry out clinical management approaches according to the disease and avoid fatal outcomes.
Article visits 1024 | PDF visits 263
- Pfefferbaum B, North CS. Mental health and the Covid-19 pandemic. N Engl J Med [Internet]. 2020;383(6):508–10. doi: https://doi.org/doi: 10.1056/NEJMp2008017
- Ritchie H, Mathieu E, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, et al. Statistics and Research Coronavirus Pandemic (COVID-19) – the data [Internet]. Our World in Data. 2021. Available from: https://ourworldindata.org/coronavirus-data
- Dunlop C, Howe A, Li D, Allen LN. The coronavirus outbreak: The central role of primary care in emergency preparedness and response. BJGP Open [Internet]. 2020;4(1):3–5. doi: https://doi.org/10.3399/bjgpopen20X101041
- Fisher D, Wilder-Smith A. The global community needs to swiftly ramp up the response to contain COVID-19. Lancet [Internet]. 2020;395(10230):1109–10. doi: https://doi.org/10.1016/S0140-6736(20)30679-6
- Instituto Nacional de Salud. Colombia. COVID-19 en Colombia Reporte 24-11-2021 5:50 p.m. 2021.
- Kluge HHP, Wickramasinghe K, Rippin HL, Mendes R, Peters DH, Kontsevaya A, et al. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet [Internet]. 2020;395(10238):1678–80. doi: https://doi.org/10.1016/S0140-6736(20)31067-9
- Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir [Internet]. 2020;8(4):e21. doi: https://doi.org/10.1016/S2213-2600(20)30116-8
- Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA - J Am Med Assoc [Internet]. 2020;323(11):1061–9. doi: https://doi.org/10.1001/jama.2020.1585
- DeBiasi RL, Song X, Delaney M, Bell M, Smith K, Pershad J, et al. Severe COVID-19 in children and young adults in the Washington, DC metropolitan region. J Pediatr [Internet]. 2020; doi: https://doi.org/10.1017/CBO9781107415324.004
- Goldstein E, Lipsitch M. Temporal rise in the proportion of younger adults and older adolescents among coronavirus disease (COVID-19) cases following the introduction of physical distancing measures, Germany, March to April 2020. Eurosurveillance [Internet]. 2020;25(17):22–5. doi: https://doi.org/10.2807/1560-7917.ES.2020.25.17.2000596
- Brodin P. Why is COVID-19 so mild in children? Acta Paediatr [Internet]. 2020;109(6):1082–3. doi: https://doi.org/10.1111/apa.15271
- Fernandes N. Economic effects of coronavirus outbreak ( COVID-19 ) on the world economy [Internet]. IESE Business School Working Paper No. WP-1240-E. 2020. doi: http://dx.doi.org/10.2139/ssrn.3557504
- Ashcroft P, Lehtinen S, Angst DC, Low N, Bonhoeffer S. Quantifying the impact of quarantine duration on covid-19 transmission. Elife [Internet]. 2021;10:1–33. doi: https://doi.org/10.7554/eLife.63704
- Wang Y, Shi L, Que J, Lu Q, Liu L, Lu Z, et al.. The impact of quarantine on mental health status among general population in China during the COVID-19 pandemic. Mol Psychiatry [Internet]. 2021;26(9):4813-4822. doi: https://doi.org/10.1038/s41380-021-01019-y
- Wood S, Harrison SE, Judd N, Bellis MA, Hughes K, Jones A. The impact of behavioural risk factors on communicable diseases : a systematic review of reviews. BMC Public Health [Internet]. 2021;21(1):1–16. doi: https://doi.org/10.1186/s12889-021-12148-y
- Gabrielli M, Franza L, Esperide A, Gasparrini I, Gasbarrini A, Franceschi F. Liver Injury in patients hospitalized for COVID-19: possible role of therapy. Vaccines. 2022;10(2):1–14. doi: https://doi.org/10.3390/vaccines10020192
- Gobbi M, Brunani A, Arreghini M, Baccalaro G, Dellepiane D, La Vela V, et al. Nutritional status in post SARS-Cov2 rehabilitation patients. Clin Nutr [Internet]. 2021; doi: https://doi.org/10.1016/j.clnu.2021.04.013
- Ceban F, Ling S, Lui LMW, Lee Y, Gill H, Teopiz KM, et al. Fatigue and cognitive impairment in Post-COVID-19 Syndrome: A systematic review and meta-analysis. Brain Behav Immun [Internet]. 2022;101(November 2021):93–135. doi: https://doi.org/10.1016/j.bbi.2021.12.020
- Puntmann VO, Carerj ML, Wieters I, Fahim M, Arendt C, Hoffmann J, et al. Outcomes of cardiovascular magnetic resonance imaging in patients recently recovered from coronavirus disease 2019 (COVID-19). JAMA Cardiol [Internet]. 2020;5(11):1265–73. doi: https://doi.org/10.1001/jamacardio.2020.3557
- Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation [Internet]. 2020;142(1):4–6. doi: https://doi.org/10.1161/CIRCULATIONAHA.120.047659
- Yang, J., Hu, J., & Zhu C. Obesity aggravates COVID‐19: a systematic review and meta-analysis. J Med Virol [Internet]. 2021;93(1):257–61. doi: https://doi.org/10.1002/jmv.26237
- Biswas M, Rahaman S, Biswas TK, Haque Z, Ibrahim B. Association of sex, age, and comorbidities with mortality in COVID-19 patients: a systematic review and meta-analysis. Intervirology [Internet]. 2021;64(1):36–47. doi: https://doi.org/10.1159/000512592
- Zhou W, Wang W. Auto-antibodies against type I IFNs are associated with severe COVID-19 pneumonia. Signal Transduct Target Ther [Internet]. 2021;6(1):2020–1. doi: http://dx.doi.org/10.1038/s41392-021-00514-6
- Aguilar F, Vega J, Suclupe D. SARS-CoV-2 : mucho más que un virus respiratorio SARS-COV-2 : more than a respiratory virus. Arch méd Camaguey [Internet]. 2021;25(2):299–315. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1025-02552021000200014&lng=es&nrm=iso
- Abebe EC, Ayele TM, Muche ZT, Dejenie TA. Neuropilin 1: A novel entry factor for sars-cov-2 infection and a potential therapeutic target. Biol Targets Ther [Internet]. 2021;15:143–52. doi: https://doi.org/10.2147/BTT.S307352
- Díaz-Casañas E, Rodríguez-Moya VS, Montes de Oca Martínez N. Surfactante pulmonar: posible intervención frente al nuevo Síndrome Respiratorio Agudo Severo Coronavirus 2 (SARS-CoV-2). Rev Habanera Ciencias Médicas [Internet]. 2020;19. Available from: http://scielo.sld.cu/scielo.php?script=sci_arttext&pid=S1729-519X2020000400016&lng=es&nrm=iso
- Yazdanpanah F, Hamblin MR, Rezaei N. The immune system and COVID-19: Friend or foe? Life Sci [Internet]. 2020;256(June):117900. doi: https://doi.org/10.1016/j.lfs.2020.117900
- Da Silveira MP, Da Silva Fagundes KK, Bizuti MR, Starck É, Rossi RC, De Resende e Silva DT. Physical exercise as a tool to help the immune system against COVID-19: an integrative review of the current literature. Clin Exp Med [Internet]. 2021;21(1):15–28. doi: https://doi.org/10.1007/s10238-020-00650-3
- Nalbandian A, Sehgal K, Gupta A, Madhavan MV., McGroder C, Stevens JS, et al. Post-acute COVID-19 syndrome. Nat Med [Internet]. 2021;27(4):601–15. doi: http://dx.doi.org/10.1038/s41591-021-01283-z
- Su Y, Yuan D, Chen DG, Ng RH, Wang K, Choi J, et al. Multiple early factors anticipate post-acute COVID-19 sequelae. Cell [Internet]. 2022;185(5):881-895.e20. doi: https://doi.org/10.1016/j.cell.2022.01.014