High-Resolution Manometry Contributions to the Physiology of Phonation
Contribuciones de la manometría de alta resolución a la fisiología de la fonación

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Show authors biography
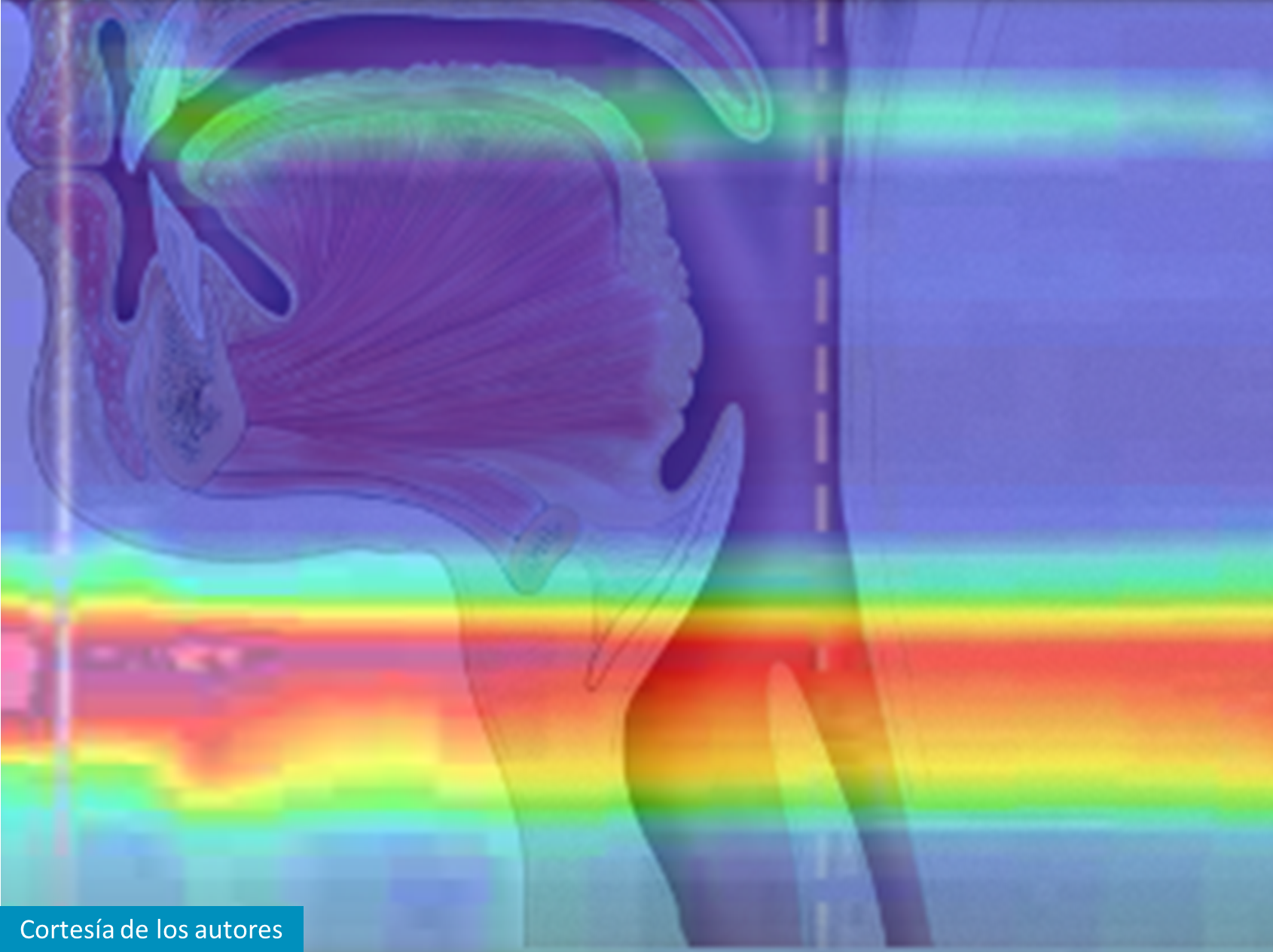
High-resolution manometry (HRM) is a motility diagnostic system that measures intraluminal pressure of the gastrointestinal tract using a series of closely spaced pressure sensors. The topographic plot generated by HRM software makes it possible to visualize phonation pressures at the pharynx, UES, and body of the esophagus in real time, indicating pressure intensity by color, which permits easy data interpretation. It has been largely used for swallowing study and dysphagia diagnosis. Due to the proximity of the pharyngoesophageal and laryngeal structures, this technology instigated voice researchers. Despite the few studies published so far, high-resolution manometry has yet proven to be an extremely useful tool in obtaining entire pharyngoesophageal segment pressure measurements during phonation. It also allows natural voice production not interfering with the mouth area. HRM data already brought light to subglottic pressure, vertical laryngeal excursion, cricopharyngeal muscle activation, air flow, muscle tension associated with vocalization and pressure variations associated with different phonatory stimuli.
Article visits 282 | PDF visits 131
- Pandolfino JE, Kahrilas PJ. AGA technical review on the clinical use of esophageal manometry. Gastroenterology [Internet]. 2005 Jan;128(1):209–24. doi: http://dx.doi.org/10.1053/j.gastro.2004.11.008
- Gyawali CP, Kahrilas PJ. A Short History of High-Resolution Esophageal Manometry. Dysphagia. 2023 Apr;38(2):586-95. doi: http://dx.doi.org/10.1007/s00455-021-10372-7
- Kahrilas PJ, Ghosh SK, Pandolfino JE. Challenging the limits of esophageal manometry. Gastroenterology. 2008 Jan;134(1):16-8. doi: http://dx.doi.org/10.1053/j.gastro.2007.11.031
- Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014 Feb;29(1):2-16. doi: http://dx.doi.org/10.1007/s00455-013-9494-5
- Jones CA, Hoffman MR, Geng Z, Abdelhalim SM, Jiang JJ, McCulloch TM. Reliability of an automated high-resolution manometry analysis program across expert users, novice users, and speech-language pathologists. J Speech Lang Hear Res. 2014 Jun 1;57(3):831-6. http://dx.doi.org/10.1044/2014_jslhr-s-13-0101
- Mielens JD, Hoffman MR, Ciucci MR, McCulloch TM, Jiang JJ. Application of classification models to pharyngeal high-resolution manometry. J Speech Lang Hear Res. 2012 Jun;55(3):892-902. doi: http://dx.doi.org/10.1044/1092-4388(2011/11-0088)
- Geng Z, Hoffman MR, Jones CA, McCulloch TM, Jiang JJ. Three-dimensional analysis of pharyngeal high-resolution manometry data. Laryngoscope. 2013 Jul;123(7):1746-53. doi: http://dx.doi.org/10.1002/lary.23987
- Omari T, Schar M. High-resolution manometry: what about the pharynx? Curr Opin Otolaryngol Head Neck Surg. 2018 Dec;26(6):382-91. doi: http://dx.doi.org/10.1097/MOO.0000000000000491
- Perera L, Kern M, Hofmann C, Tatro L, Chai K, Kuribayashi S, et al. Manometric evidence for a phonation-induced UES contractile reflex. Am J Physiol Gastrointest Liver Physiol. 2008 Apr;294(4): G885-91. doi: http://dx.doi.org/10.1152/ajpgi.00470.2007
- Vaiano T, Herbella FAM, Behlau M. Pharyngeal, upper esophageal sphincteric and esophageal pressures responses related to vocal tasks at the light of high-resolution manometry. Arq Gastroenterol. 2021;58(3): 298-301. doi: http://dx.doi.org/10.1590/s0004-2803.202100000-51
- Fry DL, Stead WW, Ebert RV, Lubin RI, Wells HS. The measurement of intraesophageal pressure and its relationship to intrathoracic pressure. J Lab Clin Med. 1952 Nov;40(5):664-73. Available from: https://www.translationalres.com/article/0022-2143(52)90002-4/pdf
- Sundberg J, Titze I, Scherer R. Phonatory control in male singing: a study of the effects of subglottal pressure, fundamental frequency, and mode of phonation on the voice source. J Voice. 1993 Mar;7(1):15-29. doi: http://dx.doi.org/10.1016/s0892-1997(05)80108-0
- Björklund S, Sundberg J. Relationship Between Subglottal Pressure and Sound Pressure Level in Untrained Voices. J Voice. 2016 Jan;30(1):15-20. doi: http://dx.doi.org/10.1016/j.jvoice.2015.03.006
- Van den Berg Jw. Direct and indirect determination of the mean subglottic pressure: Sound level, mean subglottic pressure, mean air flow, “subglottic power” and “efficiency” of a male voice for the vowel (a). Folia Phoniatr (Basel). 1956;8(1):1-24. doi: https://doi.org/10.1159/000262725
- Lieberman P. Direct comparison of subglottal and esophageal pressure during speech. J Acoust Soc Am. 1968 May;43(5):1157-64. doi: http://dx.doi.org/10.1121/1.1910950
- Kunze LH. Evaluation Of Methods Of Estimating Sub-Glottal Air Pressure. J Speech Hear Res. 1964 Jun; 7(2):151-64. doi: http://dx.doi.org/10.1044/jshr.0702.151
- Neumann K, Gall V, Schutte HK, Miller DG. A new method to record subglottal pressure waves: potential applications. J Voice. 2003 Jun;17(2):140-59. doi: http://dx.doi.org/10.1016/s0892-1997(03)00037-7
- Schutte HK, Stark JA, Miller DG. Change in singing voice production, objectively measured. J Voice. 2003 Dec;17(4):495-501. doi: http://dx.doi.org/10.1067/s0892-1997(03)00009-2
- Sundberg J, Scherer R, Hess M, Müller F, Granqvist S. Subglottal pressure oscillations accompanying phonation. J Voice. 2013 Jul;27(4):411-21. doi: http://dx.doi.org/10.1016/j.jvoice.2013.03.006
- Gyawali CP, Kahrilas PJ. A Short History of High-Resolution Esophageal Manometry. Dysphagia. 2023 Apr;38(2):586-95. doi: http://dx.doi.org/10.1007/s00455-021-10372-7
- Silva LC, Herbella FA, Neves LR, Vicentine FP, Neto SP, Patti MG. Anatomophysiology of the pharyngo-upper esophageal area in light of high-resolution manometry. J Gastrointest Surg. 2013 Dec;17(12):2033-8. doi: http://dx.doi.org/10.1007/s11605-013-2358-3
- Laurino Neto RM, Herbella FAM. A narrative review of current functional assessment of the upper esophageal sphincter. Annals of Esophagus. 2022 Sep;5: 1-5. doi: https://doi.org/10.21037/aoe-21-17
- Kahrilas PJ, Dodds WJ, Hogan WJ. Effect of peristaltic dysfunction on esophageal volume clearance. Gastroenterology. 1988 Jan;94(1):73-80. doi: http://dx.doi.org/10.1016/0016-5085(88)90612-9
- Takasaki K, Umeki H, Enatsu K, Tanaka F, Sakihama N, Kumagami H, et al. Investigation of pharyngeal swallowing function using high-resolution manometry. Laryngoscope. 2008 Oct;118(10):1729-32. doi: http://dx.doi.org/10.1097/MLG.0b013e31817dfd02
- Van Houtte E, Van Lierde K, D'haeseleer E, Van Imschoot B, Claeys S. UES pressure during phonation using high-resolution manometry and 24-h dual-probe pH-metry in patients with muscle tension dysphonia. Dysphagia. 2012 Jun;27(2):198-209. Epub 2011 Jul 7. doi: http://dx.doi.org/10.1007/s00455-011-9354-0
- Hoffman MR, Mielens JD, Ciucci MR, Jones CA, Jiang JJ, McCulloch TM. High-resolution manometry of pharyngeal swallow pressure events associated with effortful swallow and the Mendelsohn maneuver. Dysphagia. 2012 Sep;27(3):418-26. doi: http://dx.doi.org/10.1007/s00455-011-9385-6
- Knigge MA, Thibeault S, McCulloch TM. Implementation of high-resolution manometry in the clinical practice of speech language pathology. Dysphagia. 2014 Feb;29(1):2-16. doi: http://dx.doi.org/10.1007/s00455-013-9494-5
- Jones CA, Hammer MJ, Hoffman MR, McCulloch TM. Quantifying contributions of the cricopharyngeus to upper esophageal sphincter pressure changes by means of intramuscular electromyography and high-resolution manometry. Ann Otol Rhinol Laryngol. 2014 Mar;123(3):174-82. doi: http://dx.doi.org/10.1177/0003489414522975
- Vaiano T, Herbella FAM, Behlau M. High-Resolution Manometry as a Tool for Biofeedback in Vertical Laryngeal Positioning. J Voice. 2021 May;35(3):418-21. doi: http://dx.doi.org/10.1016/j.jvoice.2019.10.018
- Tanaka S, Gould WJ. Relationships between vocal intensity and noninvasively obtained aerodynamic parameters in normal subjects. J Acoust Soc Am. 1983 Apr;73(4):1316-21. doi: http://dx.doi.org/10.1121/1.389235
- Hoffmeister JD, Ulmschneider CL, Jones CA, Ciucci MR, McCulloch TM. Measurement of Pharyngeal Air Pressure During Phonation Using High-Resolution Manometry. J Speech Lang Hear Res. 2021 Sep 14;64(9):3456-64. doi: http://dx.doi.org/10.1044/2021_JSLHR-21-00005
- Hoffmeister JD, Ulmschneider CL, Ciucci MR, McCulloch TM. Stress Effects on Pharyngeal Air Pressure and Upper Esophageal Sphincter Pressure During Phonation: The Influence of Vocal Tract Semi-Occlusion. J Voice. Forthcoming 2022. doi: http://dx.doi.org/10.1016/j.jvoice.2022.07.020
- Hutcheson KA, Hammer MJ, Rosen SP, Jones CA, McCulloch TM. Expiratory muscle strength training evaluated with simultaneous high-resolution manometry and electromyography. Laryngoscope. 2017 Apr;127(4):797-804. doi: http://dx.doi.org/10.1002/lary.26397
- Ohashi M, Aoyagi Y, Ito S, Kagaya H, Hirata M, Nakata S. Comparison of electromyography, sound, bioimpedance, and high-resolution manometry for differentiating swallowing and vocalization events. Med Eng Phys. 2023 May;115:103980. doi: http://dx.doi.org/10.1016/j.medengphy.2023.103980
- Sivarao DV, Goyal RK. Functional anatomy and physiology of the upper esophageal sphincter. Am J Med. 2000 Mar 6;108(4 suppl 1):27-37. doi: http://dx.doi.org/10.1016/s0002-9343(99)00337-x
- Ranjbar PA, Maxwell PJ, Balouch B, Yam C, Alnouri G, Sataloff RT. The Relationship Between Vocal Fold Mobility Disorders and Ineffective Esophageal Motility. J Voice. Forthcoming 2023. doi: http://dx.doi.org/10.1016/j.jvoice.2023.02.016