Post-COVID-19 Laryngeal Dystonia: Report of Two Cases and Potential Pathophysiological Explanation
Distonía laríngea post COVID-19: reporte de dos casos y posible explicación fisiopatogénica

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License.
Show authors biography
Laryngeal dystonia (LD), also known as spasmodic dysphonia, is a task-specific focal movement disorder, primarily affecting voice production. The dystonic movements of the vocal folds result in a varied phenomenology, typically hard vocal breaks and strain in the adductor-type laryngeal dystonia (ADLD), and breathy breaks or aphonia in the abductor-type laryngeal dystonia (ABLD). More than 80% of patients have suffered from ADLD.
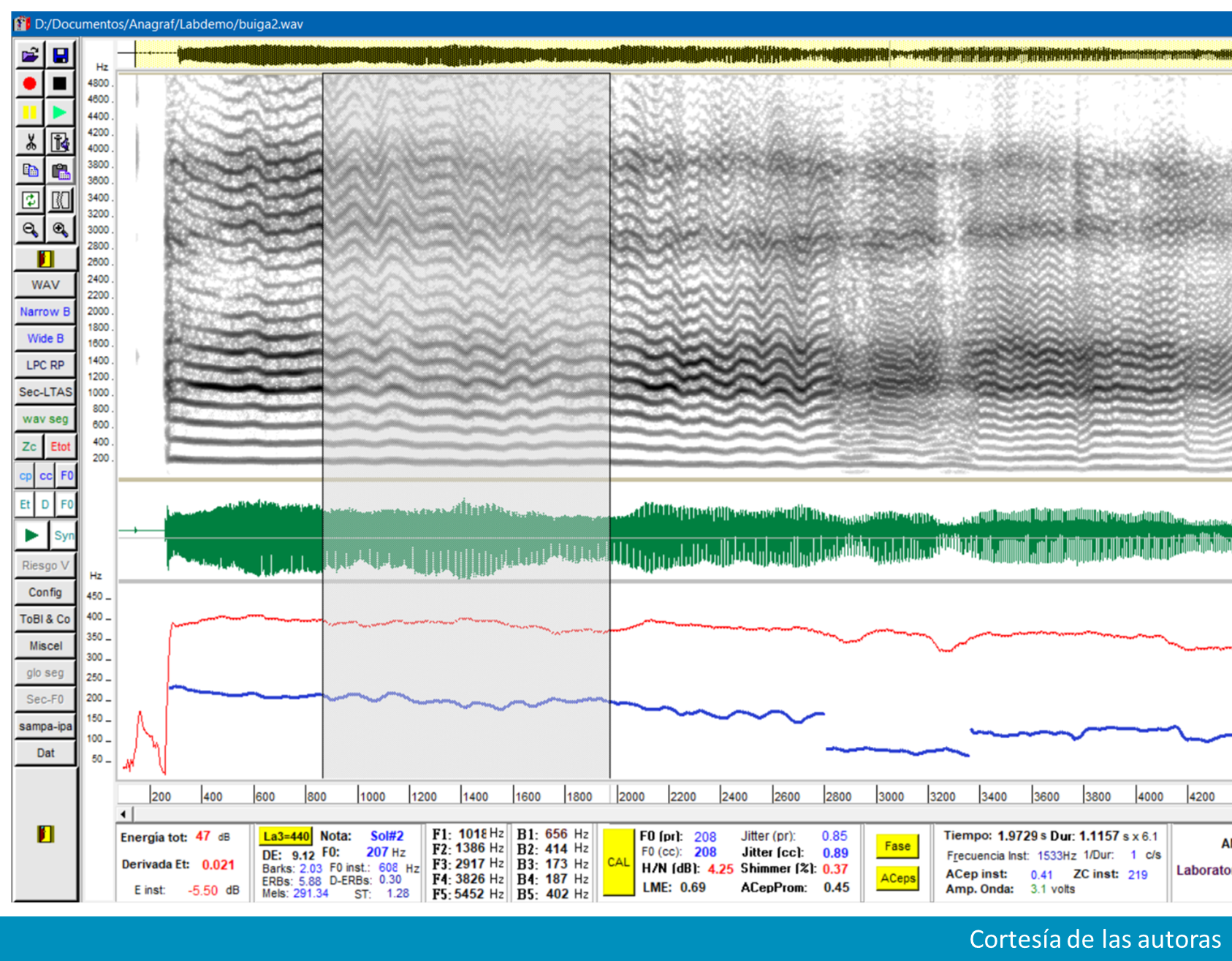
Two female patients developed LD a month after presenting an upper respiratory tract infection by COVID-19. They had the adductor-type laryngeal dystonia. Through the acoustic study of the vowel /a/ breaks, frequency changes and aperiodicity were observed. Speech was studied using the phonetogram, and the range of speech is altered in both patients.
The inflammation of the peripheral nerves of the larynx by COVID-19 produced a sensory alteration, with a maladaptive response in these patients, who perhaps had predisposing genetic basis, or the immunological activation or the invasion of the germ by retrograde pathway altered the neuronal networks involved in the genesis of LD.
Article visits 601 | PDF visits 204
- Blitzer A, Brin MF, Simonyan K , Ozelius LJ, Frucht SJ. Phenomenology, genetics, and CNS network abnormalities in laryngeal dystonia: A 30-year experience. Laringoscope [Internet]. 2018;128(51):S1-S9. doi: https://doi.org/10.1002/lary.27003 DOI: https://doi.org/10.1002/lary.27003
- Simonyan K, Barkmeier-Kraemer J, Blitzer A, Hallett M, Houde JF, Jacobson Kimberley T, et al. Laryngeal Dystonia. Multidisciplinary Update on Terminology, Pathophysiology, and Research Priorities. Neurology [Internet]. 2021;96(21):989-1001. doi: http://doi.org/10.1212/WNL.0000000000011922 DOI: https://doi.org/10.1212/WNL.0000000000011922
- Quartarone A, Hallett M. Emerging concepts in the physiological basis of dystonia. Mov Disord [Internet]. 2013;28(7):958-67. doi: http://doi.org/10.1002/mds.25532 DOI: https://doi.org/10.1002/mds.25532
- Hintze JM, Ludlow CL, Bansberg SF, Adler CH, Lott DG. Spasmodic Dysphonia: A Review. Part 2: Characterization of Pathophysiology. Otolaryngol Head Neck Surg [Internet]. 2017;157(4):558-64. doi: https://doi.org/10.1177/0194599817728465 DOI: https://doi.org/10.1177/0194599817728465
- Watts CCW, Whurr R, Nye C. (2007). Inyecciones de toxina botulínica para el tratamiento de la disfonía espasmódica. La Biblioteca Cochrane Plus [Internet]. 2004;(4). doi: https://doi.org/10.1002/14651858.CD004327.pub2 DOI: https://doi.org/10.1002/14651858.CD004327.pub2
- Barkmeier JM, Case JL, Ludlow CL. Identification of symptoms for spasmodic dysphonia and vocal tremor: A comparison of expert and nonexpert judges. J Commun Disord [Internet]. 2001;34(1-2):21-37. doi: https://doi.org/10.1016/S0021-9924(00)00039-3 DOI: https://doi.org/10.1016/S0021-9924(00)00039-3
- Edgar JD, Sapienza CM, Bidus K, Ludlow CL. Acustic measures of symptoms in abductor spasmodic dysphonia. J Voice [Internet]. 2001;15(3), 362-72. doi: http://doi.org/10.1016/S0892-1997(01)00038-8 DOI: https://doi.org/10.1016/S0892-1997(01)00038-8
- Brandão PRP, Grippe TC, Pereira DA, Munhoz RP, Cardoso F. New-Onset Movement Disorders Associated with COVID-19. Tremor and Other Hyperkinetic Movements [Internet]. 2021 Jul 8;11(1):26. doi: http://dx.doi.org/10.5334/tohm.595 DOI: https://doi.org/10.5334/tohm.595
- Chan JL, Murphy KA, Sarna JR. Myoclonus and cerebellar ataxia associated with COVID 19: a case report and systematic review. J Neurol [Internet]. 2021;268(10):3517-48. doi: http://doi.org/10.1007/s00415-021-10458-0 DOI: https://doi.org/10.1007/s00415-021-10458-0
- Elisei NG. Análisis acústico de la voz normal y patológica utilizando dos sistemas diferentes: ANAGRAF y PRAAT. Interdisciplinaria [Internet]. 2012;29(2):339-57. doi: https://doi.org/10.16888/interd.2012.29.2.9 DOI: https://doi.org/10.16888/interd.2012.29.2.9
- Gurlekian J, Molina N. Índice de perturbación, de precisión vocal y de grado de aprovechamiento de energía para la evaluación del riesgo vocal. Rev de Logop. Foniatr [Internet] 2012;32(4):156-63. doi: https://doi.org/10.1016/j.rlfa.2012.03.007 DOI: https://doi.org/10.1016/j.rlfa.2012.03.007
- Sapienza CM, Walton S, Murry T. Acoustic variations in adductor spasmodic dysphonia as a function of speech task. J Speech Lang Hear Res [Internet]. 1999;42(1):127-40. doi: http://doi.org/10.1044/jslhr.4201.127 DOI: https://doi.org/10.1044/jslhr.4201.127
- Sigal L. Disfonías Espasmódicas, estudios acústicos. Rev de Investig en Logop [Internet]. 2013;3(1):34-52. doi: https://doi.org/10.5209/rlog.58683 DOI: https://doi.org/10.5209/rlog.58683
- Sigal L. Disfonías Espasmódicas. Buenos Aires: Editorial Akadia; 2022. 220 p.
- Chhetri DK, Mendelsohn BA, Blumin JH, Berke GS. Long term flollow-up results of selective laryngeal adductor denervation-reinnervation surgery form adductor spasmodic dysphonia. Laryngoscope [Internet]. 2006;116(4):635-42. doi: https://doi.org/10.1097/01.MLG.0000201990.97955.E4 DOI: https://doi.org/10.1097/01.MLG.0000201990.97955.E4
- Whitchurch M. Adductor Spasmodic Dysphonia versus Muscle Tension Dysphonia: Exploring the precision of phonatory break analysis as a diagnostic test [master’s thesis]. Salt Lake City (UT): The University of Utah; 2008. 50 p. Available from: https://collections.lib.utah.edu/ark:/87278/s6m620v4
- Gurlekian JA, Molina N, Barmat de Mines A, Torres H, de la Arena S, Penna J. Fonetograma de la Voz Hablada: valores de referencia normal para hablantes masculinos y femeninos. 2009. Disponible en: https://es.scribd.com/document/393961920/Fonetograma-de-La-Voz-Hablada-posterUBA3-60x80
- Mahalakshmi AM, Ray B, Tuladhar S, Bhat A, Paneyala S, Patteswari D, et al. Does COVID-19 contribute to development of neurological disease?. Immun Inflamm Dis [Internet]. 2021;9(1):48-58. doi: https://doi.org/10.1002/iid3.387 DOI: https://doi.org/10.1002/iid3.387
- Brundin P, Nath A , Beckham JD. Is COVID-19 a Perfect Storm for Parkinson's Disease? Trends Neurosci [Internet]. 2020;43(12):931-3. doi: https://doi.org/10.1016/j.tins.2020.10.009 DOI: https://doi.org/10.1016/j.tins.2020.10.009
- Steardo L, Steardo L Jr, Zorec R, Verkhratsky A. Neuroinfection may contribute to pathophysiology and clinical manifestations of COVID-19. Acta Physiol [Internet]. 2020;229(3):e13473. doi: http://doi.org/10.1111/apha.13473 DOI: https://doi.org/10.1111/apha.13473
- Algahtani HA, Shirah BH, Alwaf E. Acute cervical dystonia following the BNT162b2 mRNA COVID-19 vaccine. Clin Neurol Neurosurg [Internet]. 2022;218:107304. doi: https://doi.org/10.1016/j.clineuro.2022.107304 DOI: https://doi.org/10.1016/j.clineuro.2022.107304
- Scorza FA , Scorza CA, Fiorini AC, Finsterer J. Dystonia as a complication of COVID-19 vaccinations is not as rare as portrayed. Clin Neurol Neurosurg [Internet]. 2022;222:107447. doi: http://doi.org/10.1016/j.clineuro.2022.107447 DOI: https://doi.org/10.1016/j.clineuro.2022.107447
- Grimaldi S, Lagarde S, Harlé JR, Boucraut J, Guedj E. Autoimmune Encephalitis Concomitant with SARS-CoV-2 Infection: Insight from 18F-FDG PET Imaging and Neuronal Autoantibodies. J Nucl Med [Internet]. 2020;61(12):1726-9. doi: http://doi.org/10.2967/jnumed.120.249292 DOI: https://doi.org/10.2967/jnumed.120.249292
- Marsden CD, Obeso JA, Zarranz JJ, Lang AE. The anatomical basis of symptomatic hemidystonia. Brain [Internet]. 1985;108(2),463-83. doi: https://doi.org/10.1093/brain/108.2.463 DOI: https://doi.org/10.1093/brain/108.2.463
- Jinnah HA, Neychev V, Hess EJ. The Anatomical Basis for Dystonia: The Motor Network Model. Tremor Other Hyperkinet Mov [Internet]. 2017;7:1-15. doi: https://doi.org/10.5334/tohm.383 DOI: https://doi.org/10.5334/tohm.383
- Neychev VK, Gross RE, Lehéricy S, Hess EJ, Jinnah HA. The functional neuroanatomy of dystonia. Neurobiol Dis [Internet]. 2011;42(2):185-201. doi: http://doi.org/10.1016/j.nbd.2011.01.026 DOI: https://doi.org/10.1016/j.nbd.2011.01.026
- Fuertinger S, Simonyan K. Connectome-Wide Phenotypical and Genotypical Associations in Focal Dystonia. J Neurosci [Internet]. 2017;37(31):7438-49. doi: https://doi.org/10.1523/JNEUROSCI.0384-17.2017 DOI: https://doi.org/10.1523/JNEUROSCI.0384-17.2017
- De Lima Xavier L, Simonyan K. The extrinsic risk and its association with neural alterations in spasmodic dysphonia. Parkinsonism Relat Disord [Internet]. 2019; 65:117-23. doi: https://doi.org/10.1016/j.parkreldis.2019.05.034 DOI: https://doi.org/10.1016/j.parkreldis.2019.05.034