Impact of a Workplace Vocal Health Promotion Program on Vocal Doses in College Professors: a Colombian Exploratory Study
Impacto de un programa de promoción de la salud vocal en los lugares de trabajo en las dosis vocales de los profesores universitarios: un estudio exploratorio en Colombia
Ángela Patricia Atará-Piraquive , Pasquale Bottalico, Lady Catherine Cantor-Cutiva
Abstract
Objective. To determine the effect of a workplace vocal health promotion (WVHP) program on Colombian college professors’ vocal doses. This is an exploratory pre-post-intervention study.
Methods. College professors were randomly allocated to one of two groups: no-intervention or intervention. Participants filled out a general questionnaire and were monitored using a vocal dosimeter during the complete duration of an in-person class before and after their participation in the program. The WVHP program consisted of four sessions (2 in-person and 2 online sessions; one per week) focused on vocal hygiene and training and teaching-learning strategies to be implemented inside the classrooms.
Results. The intervention group (n = 6) had a 3% decrease in time dose percentage after participating in the WVHP program, whereas professors from the no-intervention group had an increase of 1% after the follow-up (p >0.05). Participants from the no-intervention group had a statistically significant increased distance dose normalized (β = 0.078; p = 0.01) in comparison with the intervention group.
Conclusions. The WVHP program seems to be a good preventive strategy for reducing voice disorders among occupational voice users. Although statistical significance was not achieved for most vocal dose parameters, the observed trends suggest that work-based structured vocal health interventions may contribute to safer and more sustainable voice use in occupational settings.
Keywords
Vocal health promotion; voice program; working conditions; vocal doses; college professors.
Resumen
Objetivo. Determinar el efecto de un programa de promoción de la salud vocal en el lugar de trabajo (WVHP, por sus siglas en inglés) sobre las dosis vocales de profesores universitarios colombianos. Se trata de un estudio exploratorio con un diseño pre y postintervención.
Métodos. Los profesores universitarios fueron asignados aleatoriamente a uno de dos grupos: sin intervención o con intervención. Los participantes completaron un cuestionario general y fueron monitoreados con un dosímetro vocal durante la duración completa de una clase presencial, antes y después de su participación en el programa. El programa WVHP consistió en cuatro sesiones (dos presenciales y dos online, una por semana) enfocadas en higiene vocal, entrenamiento vocal y estrategias de enseñanza-aprendizaje para implementar en el aula.
Resultados. El grupo que recibió la intervención (n = 6) presentó una reducción del 3 % en el porcentaje de dosis temporal después de participar en el programa WVHP, mientras que los profesores del grupo que no recibieron la intervención mostraron un aumento del 1 % tras el seguimiento (p >0.05). Además, los participantes del grupo que no recibieron la intervención tuvieron un incremento estadísticamente significativo en la dosis de distancia normalizada (β = 0.078; p = 0.01) en comparación con el grupo que recibió la intervención.
Conclusiones. El programa WVHP parece ser una buena estrategia preventiva para reducir los trastornos de la voz en usuarios ocupacionales de la voz. Aunque no se alcanzó significancia estadística en la mayoría de los parámetros de dosis vocal, las tendencias observadas sugieren que las intervenciones estructuradas de salud vocal en el ámbito laboral pueden contribuir a un uso más seguro y sostenible de la voz en entornos ocupacionales.
Palabras clave
Promoción de la salud vocal; programa de voz; condiciones de trabajo; dosis vocales; profesores universitarios.
Introduction
Teachers have a significantly high occurrence of voice disorders due to, among other factors, a high vocal demand [1-14], which determines the speaker´s vocal demand responses [15-17]. For example, sports teachers must speak at high vocal sound pressure levels (SPL) because they teach under high background noise conditions [7,18]; kindergarten teachers may need to use a high fundamental frequency (fo) at work because their communication with kids is mainly oral [19], and younger children speak at a high pitch [16]. Kindergarten teachers’ voice use may be intense and high-pitched (both vocally distressing) for extended periods without adequate breaks due to the noisy classroom environments and the large number of pupils per classroom [20]. This suggests that teaching young children imposes a greater vocal load in terms of oscillatory cycles and distance traveled by the vocal folds [16]. Similarly, college professors face work-related vocal challenges, including background noise (often increasing their loudness and pitch), room size, audience, the task of lecturing [21-23], and working in more than one university at the same time [21], which implies more hours of vocal use in different challenging rooms.
Vocal demand response (vocal load) can be quantified using the analysis of the acoustic signal in vocal dose measures [24]. These measures include time dose (i.e., total phonation time), cycle dose (i.e., total vocal fold vibration cycles), distance dose (i.e., total distance covered by the vocal folds), energy dissipation dose (i.e., the total amount of heat generated by the vocal folds), and radiated energy dose (i.e., the total energy emitted by the mouth) [25-27]. Although previous research has quantified vocal doses of teachers [7,15,16,27], few studies have used these measures to assess the effect of voice intervention programs [28,29] such as the use of vocal amplification in classrooms. A previous study found a significant decrease in mean vocal intensity of 7dB SPL (P<0.001) using amplification, along with significant decreases (P-value=0.001) in cycle dose and distance dose [29].
Considering that college professors have a high vocal demand response [30], healthy occupational voice use among these workers should be a priority for the Departments of Education and Occupational Health. Among the options for interventions at work, Workplace Vocal Health Promotion (WVHP) programs are recommended for improving occupational voice use among college professors because this approach focuses on improving the working organization and working environment, increasing workers' participation in the adjustments of the working conditions inside the classrooms. With this in mind, this study aimed to assess the effect on vocal doses of a WVHP program implemented among college professors. In addition, we analyzed whether age, years of experience, and the number of students (working conditions) affect the relationship between the WVHP program and vocal doses among college professors.
Methods
Design and Participants
This was an exploratory longitudinal study with a pre-post measurement design. The total duration of this study was six weeks, with vocal dosimetry assessments conducted during both the pre-intervention phase in the first week and the post-intervention phase in the last week. The participants attended weekly sessions (1 per week) for four weeks. Ten college professors agreed to participate in this study and were divided into two groups: an intervention group and a no-intervention group. For this study, we used basic balanced randomization with numerical coding to assign participants to each group [31]. To be included in the study, participants had to be actively employed as college professors at the university and have had no prior participation in voice therapy or structured vocal training programs within the last three years. This restriction was implemented to ensure that any observed effects could be attributed to the intervention rather than prior training experiences. Additionally, eligible professors were required to have a teaching schedule that did not exceed six hours of in-person lectures per day (continuous or distributed throughout the day), allowing for a relatively uniform vocal workload across participants.
In order to make the sample of participants more comparable, voice dosimetry was conducted during the first class of the day for each participant (ranging from 120 to 240 minutes). This approach helped minimize variability due to potential cumulative vocal load. For most participants, the monitored class lasted approximately two hours. All participants agreed to take part in all phases of the study, including vocal dosimetry monitoring and self-reported surveys on working conditions.
Professors with chronic or recurrent respiratory conditions, such as untreated allergies or gastroesophageal reflux disease, were not eligible to participate, as these conditions can influence vocal function. Faculty members with a history of surgeries involving the neck, chest, or vocal folds were also excluded to prevent confounding variables related to post-surgical vocal adaptations. However, participants who reported occasional voice discomfort or mild symptoms were not excluded, as long as they were not actively seeking medical treatment at the time of the study. This decision was made to ensure that the sample reflected real-world variability in occupational voice use among college professors.
Before beginning the study, all participants provided written informed consent, acknowledging their voluntary participation and understanding of the research process. The study adhered to ethical research standards and received approval from the Institutional Research Ethics Committee (Approval Code 011-19). Other results from different data analyzed from this research have been published previously in Atará-Piraquive et al [32].
Voice dosimetry
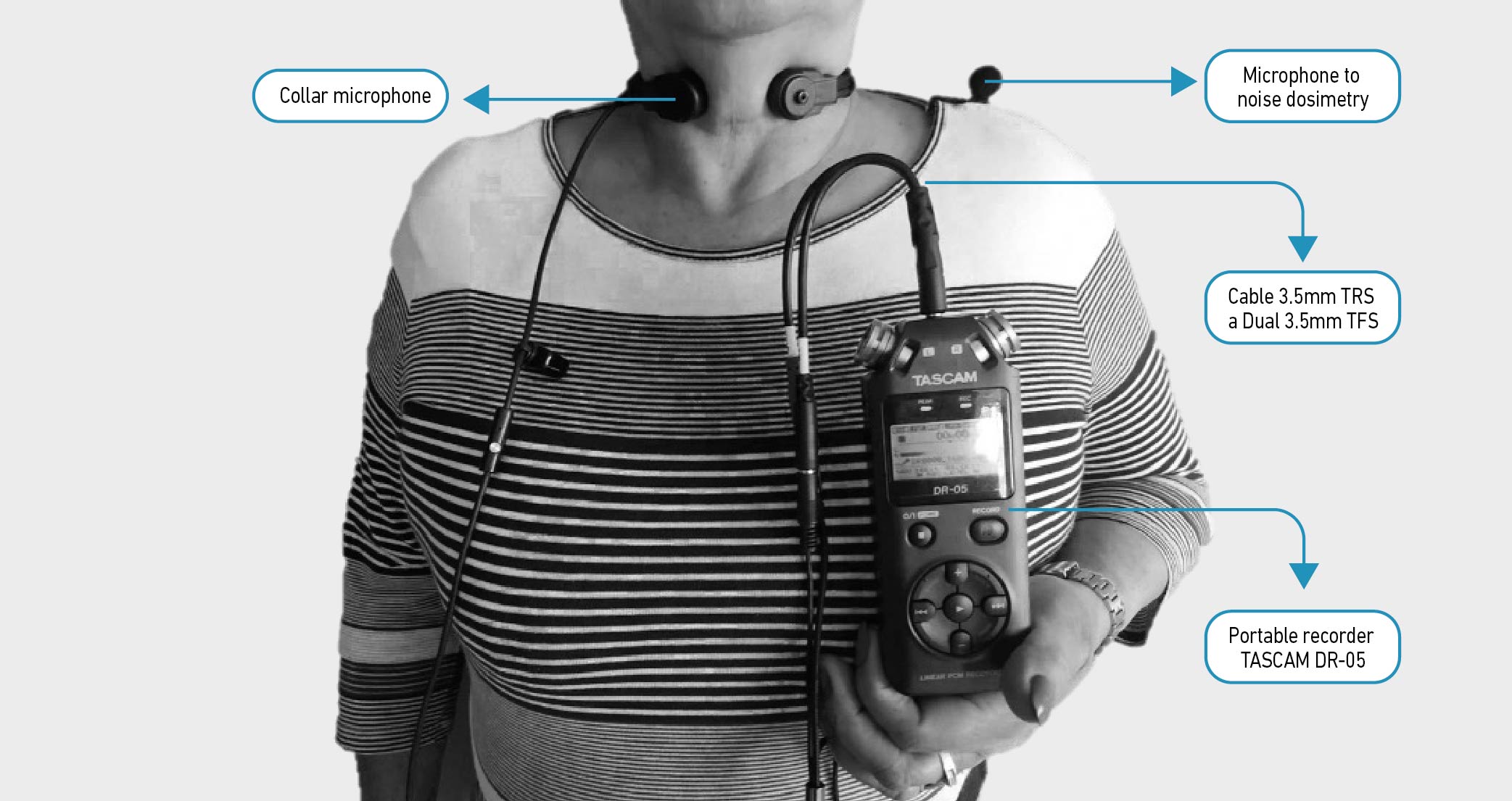
Voice dosimetry was performed using a voice dosimeter build with a collar microphone [33], and a portable recorder (TASCAM DR-05) (Figure 1). Calibrations were performed at the lab of Occupational Health. This laboratory contains a sound booth and other instrumentation for individual and environmental measurements in working settings. The second author, who holds a master’s degree in Telecommunications Engineering, trained the first author in the microphone calibration process and how to perform the voice dosimetry. During the calibration process, participants were asked to produce a sustained vowel /a/ from their softest to their loudest voice (in four levels of loudness). At the same time, a reference microphone (Audiotechnica-3350) was positioned 10 cm from the participants’ mouths to correlate the level to the SPL with a sound level meter (Smart Sensor As824). After the calibration, the data were saved to an SD card and analyzed to estimate the relationship between the signal at the microphone's output and the SPL [25,34,35]. The recorder was set to a sampling rate of 44.1 kHz. The signals were processed with the software MATLAB R2020b (MathWorks, Natick, MA). Each device was adjusted based on standardized calibration protocols, and the vocal dosimeter was individually calibrated to each subject's sound pressure level (SPL) range from the throat microphone. This calibration process ensured that variations in SPL detection were accounted for, providing reliable and personalized measurements for each participant.
Figure 1. Voice dosimeter.
Questionnaire
Participants filled in a "Voice-related working conditions questionnaire” which included four sections: (1) Sociodemographic information including age, gender, marital status, and teaching category, (2) health conditions associated with voice symptoms, such as colds, laryngitis, rhinitis, sinus infections, thyroid problems, respiratory allergies, and gastroesophageal reflux, (3) Working conditions including experience, classes per week, hours per day, students on average, self-reported background noise, acoustic conditions, temperature changes, dust and exposure to chemical conditions. Responses were recorded on a ten-point Likert scale, ranging from 0 ("Never") to 10 ("Always"), to indicate the frequency of specific conditions in their work environment and (4) Voice symptoms like hoarseness, vocal fatigue, and throat pain. For this manuscript, five questions were included in the analysis: Age, years of Experience, number of students per class, number of weekly classes, and daily hours of teaching.
Workplace Vocal Health Promotion (WVHP) program
The WVHP program consisted of four sessions, each lasting 45 minutes, spread across four weeks. Participants engaged in one session per week, with a combination of two in-person meetings and two virtual lessons delivered via the Moodle platform [36]. The first and last sessions were conducted in person and developed by a speech-language pathologist with seven years of experience in voice therapy (first author). The second and third sessions were online and delivered using the platform Moodle. The program was designed to integrate easily into the participants' routines while ensuring effective learning and practice. The complete program contained three “conceptual” modules: vocal hygiene, vocal training, and workflow modifications to reduce vocal load in the classroom.
• Vocal Hygiene Strategies: This component provided participants with practical guidance on maintaining vocal health, including hydration techniques, minimizing harmful vocal behaviors, and optimizing their speaking environments to prevent phonotrauma [37,38].
• Vocal Training: This module provided participants with exercises aimed at improving vocal efficiency and minimizing strain. The training included techniques for posture optimization, breath support, and phonation control. Participants engaged in structured warm-up and cool-down routines, articulation exercises, and resonance training. Additional emphasis was placed on voice projection strategies that enhance clarity while reducing vocal effort. Practical application exercises were incorporated to ensure the transfer of learned techniques into daily occupational voice use [38-49]. Each participant received a personalized home-based exercise plan to reinforce the content of each session. The plan included short, easy-to-follow routines designed to be implemented before and during teaching activities. Participants were encouraged to integrate these exercises into their daily work schedule, particularly before entering the classroom and when possible during class transitions, as a strategy to promote consistent vocal care in real occupational settings.
• Workplace Adaptations on Teaching-Learning Process: This section introduced professors to strategies that reduce vocal demand responses during teaching. Participants received information on classroom management techniques, effective use of non-verbal communication, and integration of multimedia and digital resources to decrease vocal demands during teaching. Teachers were trained in classroom design for safe occupational voice use (to avoid speaking from long distances), incorporation of pre-recorded videos, digital whiteboards, and projected content to minimize their vocal demand response. They also received recommendations on basic voice amplification tools and practical advice to improve classroom acoustic conditions, such as keeping windows closed and avoiding reverberant environments. In addition, the program promoted the use of supporting digital tools such as Google Classroom for content management, Canva to create infographics, GoConqr for developing interactive materials, and digital mind maps to organize the lesson content. These tools were introduced as effective strategies to diversify the content delivery, reduce vocal demand, and foster a safer occupational voice use during teaching.
The participants in the no-intervention group did not have access to the materials of the WVHP program during the duration of the study. However, they were granted access to the materials after the research was finished. To reinforce learning and encourage practice, participants in the intervention group followed a structured self-guided routine, performing exercises twice per day and three times per session. More information on the development of the WVHP program is published in Atará-Piraquive et al. [32].
Data collection procedures
Pre- monitoring phase
At baseline, the pre-intervention assessment was performed in the Occupational Health Lab before each teacher´s class. Each participant filled in a consent form and the Voice-related working conditions questionnaire. The first author conducted the voice assessment. The voice dosimeter was calibrated and set up for all participants before their first class of the day. The voice assessment included voice recordings (vowel and reading) and hearing screening. More detailed information on these procedures is described in a previous publication [32].
Teacher´s class monitoring
Participants were monitored through a voice dosimeter (collar microphone + portable recorder TASCAM DR-05) before and after a four-week WVHP program. Before the monitoring, participants met with the first author and set up the voice dosimeter. Then, the calibration process was performed, and the first author walked with the participant to their classroom, where the monitoring started. The voice dosimeter was unobtrusive and lightweight enough (289 gr) to allow the participant to engage in a normal teaching class. At the end of the class, the professor returned to the laboratory to deliver the equipment and perform the post-monitoring voice assessment. To assess vocal load during teaching sessions, various vocal dose measures were extracted, including distance dose-normalized (Dd_n), energy dissipation dose-normalized (De_n), and radiated energy dose-normalized (Dr_n). Additionally, the Vocal Loading Index (VLI) was calculated as another measure of cumulative vocal exposure over time by integrating phonation time, fundamental frequency (fo), and sound pressure level (SPL) [25]. This measure provides additional insight into the overall vocal demands experienced by teachers during their workday.
Post-monitoring phase
Immediately after class monitoring, participants returned to the lab and performed the same voice assessment protocol. The monitoring had an average duration of 4 hours (ranging between 2 and 4) per teacher.
Four weeks later, after finishing the WVHP program, participating teachers returned to the lab and underwent the same assessment protocol (pre-monitoring assessment, class monitoring, and post-monitoring assessment). The participating teachers were requested to teach similarly structured classes during the monitoring days to facilitate comparison.
In line with the research question of this manuscript, our results are based on the first pre-monitoring assessment (pre-intervention) and the last post-monitoring assessment (post-intervention).
Statistical analysis
For this study, the dependent variables (vocal doses) were defined as follows: time dose (Dt), cycle dose (Dc), distance dose (Dd), dissipation-energy dose (De), and radiated-energy dose (Dr). The vocal doses Dd, De, and Dr were normalized to the time dose Dt (Distance Dose normalized, Dissipation-Energy dose normalized, and Radiated-Energy Dose normalized). These normalized doses express the amount of exposure per second of continuous voiced speech, excluding unvoiced segments [50].
For the statistical analysis, the normality of the distribution was assessed using the Shapiro-Wilk test. Then, since the sample size was small (n = 10), we used the Wilcoxon signed-rank test to evaluate the effect of vocal doses between the before and after the intervention for both groups. The difference in vocal doses between the intervention and no-intervention groups was assessed using the Mann-Whitney U Test. In addition, we assessed the association of age, years of teaching experience, and the number of students in classes with teachers´ vocal doses using generalized estimating equations (GEEs). All the significance levels were established at p<0.05. We assessed the association between vocal doses and these independent variables (age, years of teaching experience, and number of students per class) to evaluate the potential confounding effects of previously reported associated factors of voice disorders. SPSS Statistics version 24 (IBM Corporation) was used for all statistical analyses.
Results
Sociodemographic information
A total of 10 professors participated in this study. Participants in the intervention group (n = 6) were 4 males and 2 females, whereas in the no-intervention group (n = 4), there were 2 male participants and 2 females. On average, professors from the intervention group were 35 years old (SE = 3), whereas professors from the no-intervention group were 49 years old (SE = 8), as seen in Table 1.
Table 1. General characteristics of participants per group.
| Variable | Intervention (n=6) | No intervention (n=4) | ||
|---|---|---|---|---|
| Mean | SE | Mean | SE | |
| Age | 35 | 3 | 49 | 8 |
| Experience | 8 | 2 | 16 | 5 |
| Number of Students per Class | 43 | 10 | 37 | 8 |
| Number of weekly classes | 3 | 0.4 | 4 | 0.9 |
| Daily hours of teaching | 4.0 | 0.7 | 3.5 | 0.3 |
Self-reported working conditions
Participating teachers taught a class with an average duration of 4 hours (ranging between 2 and 6). Participants from the intervention group had fewer years of experience (mean = 8; SE = 2), more students per class (n = 43; SE = 10), smaller class load per week (n = 3), and more teaching hours per day (mean = 4) compared with participants in the no-intervention group who had an average of 16 years of experience (SE = 5), 37 students per class (SE = 8), 4 classes per week, and 3.5 teaching hours per day (Table 1). Although these differences were not statistically significant, the researchers decided to analyze whether there was an association of these variables with the vocal doses to avoid potential bias.
Effect of a WVHP program, individual and work-related conditions on Colombian College Professors' Vocal Doses
The results suggest that none of the vocal dose measures were statistically significantly different between the groups before the intervention (p > 0.05 for all variables; Mann-Whitney U Test). There was no statistically significant difference in the time dose (Dt_p) for either group when comparing the results before and after the intervention. However, there was a decrease in time dose for those in the intervention group of 3% (p>0.05, Wilcoxon signed-rank test; β = -0.21, p = 0.28 GEEs) and an increase in time dose for those in the no-intervention group of 1% (p>0.05, Wilcoxon signed-rank test). At the end of this study, participants from the no-intervention group registered a non-statistically significant reduced VLI difference (p >0.05, Wilcoxon signed-rank test; β= -0.235, p=0.46 GEEs) and increased Radiated-Energy Dose normalized (p >0.05, Wilcoxon signed-rank test) compared to the intervention group. Participants from the no-intervention group had a statistically significant increased Distance Dose normalized (p=0.08, Wilcoxon signed-rank test; β = 0.078 p = 0.01 GEEs) and a non-statistically significant increased Dissipation-Energy dose normalized (p >0.05, Wilcoxon signed-rank test; β = -0.182 p = 0.69 GEEs) in comparison with the intervention group (Tables 2 and 3).
Table 2. Distribution of characteristics per group and moments of measurement.
| Variable | Intervention (n=6) | No Intervention (n=4) | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre | Post | Pre | Post | p-value Wilcoxon test | ||||||
| Mean | SE | Mean | SE | p-value Wilcoxon test | Mean | SE | Mean | SE | ||
| Dt_p | 38.56 | 3.65 | 35.96 | 3.80 | 0.063 | 45.12 | 8.72 | 46.46 | 9.03 | 0.361 |
| VLI | 429.49 | 76.18 | 387.47 | 84.29 | 0.128 | 536.21 | 157.34 | 500.16 | 176.07 | 0.464 |
| Dd_norm | 4.21 | 0.20 | 4.09 | 0.19 | 0.866 | 3.66 | 0.17 | 3.87 | 0.25 | 0.008* |
| De_norm | 35.41 | 7.80 | 32.71 | 7.87 | 0.866 | 20.81 | 5.87 | 27.18 | 10.78 | 0.692 |
| Dr_norm | 5445.43 | 998.81 | 6977.81 | 2443.93 | 0.310 | 3747.03 | 1431.16 | 4138.53 | 1125.22 | 0.131 |
Note. SE= Standard Error; Dt_p=Time dose (%); VLI= Vocal Loading Index; Dd_norm=Distance dose-normalized; De_norm= energy dissipation dose-normalized; Dr_norm= radiated energy dose-normalized
Table 3. GEEs of vocal doses with independent variables (Intervention, age, experience, and number of students).
| Intervention (yes/no) | Age | Experience | Number of students | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | p-value | Beta | SE | p-value | Beta | SE | p-value | Beta | SE | p-value | |
| Dt_p* | -0.21 | 0.19 | 0.28 | 0.01 | 0.01 | 0.26 | 0.02 | 0.01 | 0.05 | 0.00 | 0.00 | 0.49 |
| VLI | -0.24 | 0.33 | 0.47 | 0.01 | 0.01 | 0.30 | 0.04 | 0.02 | 0.06 | 0.01 | 0.01 | 0.31 |
| Dd_norm* | 0.10 | 0.04 | 0.02 | 0.00 | 0.00 | 0.13 | -0.01 | 0.00 | 0.12 | 0.00 | 0.00 | <.001 |
| De_norm | 0.35 | 0.36 | 0.33 | -0.01 | 0.01 | 0.68 | -0.03 | 0.03 | 0.31 | -0.01 | 0.01 | 0.07 |
| Dr_norm* | 0.46 | 0.30 | 0.13 | 0.00 | 0.01 | 0.68 | -0.01 | 0.02 | 0.54 | -0.01 | 0.01 | <.001 |
Note. * Variable with a p-value <0.05 in one of the independent variables.
Effect of age, years of teaching experience, and number of students on Colombian college professors' vocal doses
As shown in Table 3, there was an increased time dose (Dt_p) in more experienced teachers compared with their colleagues with fewer years of experience (p = 0.05). Likewise, the participants who had higher values of Distance Dose normalized had more students in the classrooms (p = 0.00), and subjects with higher Radiated-Energy Dose normalized values reported a smaller number of students in the class (p=0.00).
Discussion
This study aimed to assess the effect of a WVHP program on vocal doses in college professors, showing three key findings. First, participants in the intervention group showed a trend towards decreased VLI and increased Distance Dose normalized, Dissipation-Energy dose normalized, and Radiated-Energy Dose normalized compared to their colleagues in the no-intervention group. Second, a statistically significant difference in Distance Dose normalized post the WVHP program between the groups was observed. Third, higher time doses were associated with more years of experience, while Distance Dose normalized and radiated energy Dose normalized were linked to the number of students per class.
At baseline, vocal time dose in percentage (Dt_p) ranged from 38% for professors in the intervention group to 45% for those in the no-intervention group, highlighting the substantial vocal demand placed on college professors compared to primary school or music teachers [17]. Following the WVHP program, a modest 3% average reduction in Dt_p for professors in the intervention group was noted, though not statistically significant. Although the differences were not statistically significant, the observed trend suggests a potential positive impact on vocal demand response, with a reduction in the duration of occupational voice use that could help mitigate vocal fold damage caused by collision forces [6,7]. Nonetheless, caution is warranted, and further studies are needed to confirm the effectiveness of workplace vocal health promotion programs. Although direct comparisons with similar studies are challenging, previous research on voice amplification systems in primary schools and kindergartens also reported no significant effect on Dt_p [28,51].
Concerning distance dose normalized, the intervention group exhibited a decrease in this parameter, while the no-intervention group showed a statistically significant, though small, increase. GEE analysis revealed that teachers from the intervention group had a slightly higher (Beta= 0.10) dose compared to their counterparts in the no-intervention group. Interestingly, our findings suggest that college professors experience a greater amount of vocal fold vibration, posing a higher risk of damage due to collision forces compared to other teacher groups, such as primary school teachers (Dd_norm = 0.72 for females and Dd_norm = 0.48 for males) [50].
Participants from the no-intervention group displayed a more substantial increase in Dissipation-Energy dose normalized by the end of the study; however, this change was not statistically significant. Elevated values of this parameter could be linked to higher voice SPL values [7], indicating potentially increased vocal loudness, effort, and fatigue. However, this association was not evaluated in our study, and future research is needed to confirm this hypothesis.
Our results suggest that teachers in the intervention group may lean towards a more resonant voice as a result of the WVHP program, as evidenced by higher values in Radiated-Energy Dose normalized at the end of the study compared to baseline measures, although an increase was observed in the intervention group, this change was not statistically significant. Given that the Radiated-Energy Dose normalized quantifies the total energy radiated in the mouth, representing sound power when a talker is considered a sound source [50], this interesting result warrants exploration in future research.
Despite the absence of statistically significant changes in most vocal doses post-implementation of the program, a consistent tendency towards reduced vocal demand response, especially in Distance Dose normalized and Time dose, was observed. These doses are crucial as they may be related to the recovery effect of voicing pauses [50]. These findings agree with Atará-Piraquive et al., who noted a tendency to decrease jitter and shimmer after implementing an online Workplace Vocal Health and Low-Stress Levels (WVHLS) Promotion Program among college professors [52]. Vocal demand parameters are known to influence the modulation over time of various voice parameters, such as jitter, shimmer, loudness, pitch variability, formant transitions, speaking rate, and articulation rate [24]. Understanding the normal variability of vocal dose measures is essential to determining the clinical relevance of observed changes. In previous research, natural fluctuations in Distance Dose, Dissipation-Energy Dose, and Radiated-Energy Dose have been reported among occupational voice users, with daily variations influenced by workload, teaching style, and environmental factors [27]. Although no statistically significant differences were found in this study, the magnitude of change in some parameters suggests that further exploration is needed. For example, while the no-intervention group showed a statistically significant increase in Distance Dose normalized, the small decrease in the intervention group may still indicate a trend toward reduced vocal effort. Establishing normative thresholds for variability in these measures would be beneficial in future research to determine whether observed changes fall within expected ranges or indicate meaningful effects of intervention strategies.
Additionally, Cantor-Cutiva et al., implementing a Three-Week WVHP, found statistically significant decreases in fundamental frequency, standard deviation of fundamental frequency, sound pressure levels, and SPL standard deviation among both pupils and their teacher, indicating potential improvements in voice production and reduction of vocal fatigue [53]. Therefore, we hypothesize that participants in such work-related interventions, like the WVHP program, adjust their voice use, considering their class settings, leading to reduced vocal effort. Future studies are recommended to confirm this hypothesis.
As a final recommendation, our results suggest that interventions in occupational voice should encompass strategies following the hazard control hierarchy, including adjustments in the working conditions. Moreover, online programs with synchronous and asynchronous sessions can be effective alternatives for college professors, facilitating participation without disrupting their schedules [54]. Prioritizing activities to reduce stress levels and voice symptoms in workplace health promotion programs implemented in educational settings is crucial [55]. Karjalainen et al. implemented a voice program focusing on classroom communication, resulting in significant improvements, reduced voice problems, lower stress scores, and higher self-efficacy [56].
Despite limitations like a small sample size and the exclusion of schoolteachers, the exploratory nature and methodological rigor of this research minimize the likelihood of bias. While our results showed that participants in the intervention group were younger and less experienced, potentially introducing bias, the balanced block randomization mitigates this concern.
Legislation regarding occupational voice plays a critical role in safeguarding the health and well-being of workers, especially in environments where vocal demands are significant. However, several countries worldwide do not recognize voice disorders as an occupational disease [57], being the United States among these [58]. However, adherence to ergonomic standards, as outlined by the Occupational Safety and Health Administration (OSHA), not only ensures the physical comfort of workers but also aids in preventing voice disorders among teachers. OSHA categories include safety hazards, work organization hazards (such as increased hours of vocal use), physical hazards (such as exposure to noisy or dusty environments), and ergonomic hazards (such as poor posture), all of which could potentially pose risks to vocal functioning. In countries like Brazil, Chile, and Colombia in South America, while regulations acknowledge the "occupational nature" of voice disorders among teachers and other occupational voice users, practical implementation often requires adjustments, as highlighted by Mello et al. [57].
One of the primary challenges within formal health systems is that some physicians lack the necessary training and expertise to determine whether medical conditions, such as voice disorders, may be linked to occupational factors. This issue often arises from a lack of understanding of workplace risks that might impact vocal health, such as exposure to environmental irritants or high vocal demands. Consequently, occupational voice users experiencing voice disorders may not receive appropriate evaluation or management strategies tailored to address potential workplace-related causes. Bridging the gap in occupational health awareness and education within the medical community is essential for healthcare professionals to address workplace-related health concerns, including vocal health, effectively. Legal frameworks should also guide appropriate rest periods, breaks, and workload distribution, all of which are vital for maintaining vocal health and preventing occupational voice problems. Furthermore, recent scientific endeavors to establish occupational safety criteria for vocalization underscore the importance of such developments [33].
Conclusion
The results of this study suggest that the WVHP program seems to be a good preventive strategy for reducing voice disorders among occupational voice users. Although statistical significance was not achieved for most vocal dose parameters, the observed trends suggest that work-based structured vocal health interventions may contribute to safer and more sustainable voice use in occupational settings.
References
1. Bottalico P, Astolfi A, Hunter EJ. Teachers’ voicing and silence periods during continuous speech in classrooms with different reverberation times. J Acoust Soc Am [Internet]. 2017;141(1):EL26-EL31. doi: https://doi.org/10.1121/1.4973312
2. Calosso G, Puglisi GE, Astolfi A, Castellana A, Carullo A, Pellerey F. A one-school year longitudinal study of secondary school teachers’ voice parameters and the influence of classroom acoustics. J Acoust Soc Am [Internet]. 2017;142(2):1055-66. doi: https://doi.org/10.1121/1.4998707
3. Cantor-Cutiva LC, Puglisi GE, Astolfi A, Carullo A. Four-day Follow-up Study on the Self-reported Voice Condition and Noise Condition of Teachers: Relationship Between Vocal Parameters and Classroom Acoustics. J Voice [Internet]. 2017;31(1):120.E1-120.E8. doi: https://doi.org/10.1016/j.jvoice.2016.02.017
4. Gama ACC, Santos JN, Pedra EFP, Rabelo ATV, Magalhaes MC, Casas EBL. Vocal dose in teachers: correlation with dysphonia. CoDAS [Internet]. 2016;28(2):190-2. doi: https://doi.org/10.1590/2317-1782/20162015156
5. Mehta DD, Van Stan JH, Hillman RE. Relationships between vocal function measures derived from an acoustic microphone and a subglottal neck-surface accelerometer. IEEEACM Trans Audio Speech Lang Process [Internet]. 2016;24(4):659-68. doi: https://doi.org/10.1109/TASLP.2016.2516647
6. Mozzanica F, Selvaggio A, Ginocchio D, Pizzorni N, Scarponi L, Schindler A. Speech and Language Pathologists’ Voice Use in Working Environments: A Field Study Using Ambulatory Phonation Monitoring. Folia Phoniatr Logop [Internet]. 2017;68(6):268-73. doi: https://doi.org/10.1159/000481884
7. Nusseck M, Richter B, Spahn C, Echternach M. Analysing the vocal behaviour of teachers during classroom teaching using a portable voice accumulator. Logoped Phoniatr Vocol [Internet]. 2018;43(1):1-10. doi: https://doi.org/10.1080/14015439.2017.1295104
8. Pirila S, Pirila P, Ansamaa T, Yliherva A, Sonning S, Rantala L. Relationship between Activity Noise, Voice Parameters, and Voice Symptoms among Female Teachers. Folia Phoniatr Logop [Internet]. 2018;69(3):94-102. doi: https://doi.org/10.1159/000484204
9. Puglisi GE, Astolfi A, Cantor Cutiva LC, Carullo A. Four-day-follow-up study on the voice monitoring of primary school teachers: Relationships with conversational task and classroom acoustics. J Acoust Soc Am [Internet]. 2017;141(1):441-52. doi: https://doi.org/10.1121/1.4973805
10. Rabelo ATV, Santos JN, Souza BO, Gama ACC, Castro Magalhães M. The Influence of Noise on the Vocal Dose in Women. J Voice [Internet]. 2019;33(2):214-9. doi: https://doi.org/10.1016/j.jvoice.2017.10.025
11. Schloneger MJ, Hunter EJ. Assessments of Voice Use and Voice Quality Among College/University Singing Students Ages 18-24 Through Ambulatory Monitoring with a Full Accelerometer Signal. J Voice [Internet]. 2017;31(1):124.E21-124.E30. doi: https://doi.org/10.1016/j.jvoice.2015.12.018
12. Szabo Portela A, Granqvist S, Ternström S, Södersten M. Vocal Behavior in Environmental Noise: Comparisons Between Work and Leisure Conditions in Women with Work-related Voice Disorders and Matched Controls. J Voice [Internet]. 2018;32(1):126.E23-126.E38. doi: https://doi.org/10.1016/j.jvoice.2017.04.010
13. Vilkman E. Voice problems at work: A challenge for occupational safety and health arrangement. Folia Phoniatr Logop [Internet]. 2000;52(1-3):120-5. doi: https://doi.org/10.1159/000021519
14. Whitling S, Lyberg-Åhlander V, Rydell R. Long-Time Voice Accumulation During Work, Leisure, and a Vocal Loading Task in Groups with Different Levels of Functional Voice Problems. J Voice [Internet]. 2017;31(2):246.E1-246.E10. doi: https://doi.org/10.1016/j.jvoice.2016.08.008
15. Morrow SL, Connor NP. Comparison of Voice-Use Profiles Between Elementary Classroom and Music Teachers. J Voice [Internet]. 2011;25(3):367-72. doi: https://doi.org/10.1016/j.jvoice.2009.11.006
16. Remacle A, Morsomme D, Finck C. Comparison of Vocal Loading Parameters in Kindergarten and Elementary School Teachers. J Speech Lang Hear Res [Internet]. 2014;57(2):406-15. doi: https://doi.org/10.1044/2013_JSLHR-S-12-0351
17. Atará-Piraquive AP, Cantor-Cutiva LC. Gender differences in vocal doses among occupational voice users: a systematic review of literature and meta-analysis. Logoped Phoniatr Vocol [Internet]. 2022(1);63-72. doi: https://doi.org/10.1080/14015439.2021.1873415
18. Kristiansen J, Lund SP, Persson R, Shibuya H, Nielsen PM, Scholz M. A study of classroom acoustics and school teachers’ noise exposure, voice load and speaking time during teaching, and the effects on vocal and mental fatigue development. Int Arch Occup Environ Health [Internet]. 2014;87(8):851-60. doi: https://doi.org/10.1007/s00420-014-0927-8
19. Munier C, Brockmann-Bauser M, Laukkanen AM, Ilomäki I, Kankare E, Geneid A. Relationship Between Laryngeal Signs and Symptoms, Acoustic Measures, and Quality of Life in Finnish Primary and Kindergarten School Teachers. J Voice [Internet]. 2020;34(2):259-71. doi: https://doi.org/10.1016/j.jvoice.2018.12.006
20. Darius S, Voigt-Zimmermann S, Böckelmann I. Effects of occupation-specific vocal stress on the mental health of day care teachers. Folia Phoniatr Logop [Internet]. 2023;75(5):306-15. doi: https://doi.org/10.1159/000530283
21. Cantor-Cutiva LC, Robles-Vega HY, Sánchez EA, Morales DA. Differences on Voice Acoustic Parameters between Colombian College Professors with and without Vocal Fatigue. J Voice [Internet]. 2022;36(2):219-25. doi: https://doi.org/10.1016/j.jvoice.2020.05.008
22. Higgins KP, Smith AB. Prevalence and Characteristics of Voice Disorders in a Sample of University Teaching Faculty. CICSD [Internet]. 2012;39(Fall):69-75. doi: https://doi.org/10.1044/cicsd_39_F_69
23. Kyriakou K, Petinou K, Phinikettos I. Risk Factors for Voice Disorders in University Professors in Cyprus. J Voice [Internet]. 2018;32(5):643.E1-643.E9. doi: https://doi.org/10.1016/j.jvoice.2017.07.005
24. Hunter EJ, Cantor-Cutiva LC, van Leer E, van Mersbergen M, Nanjundeswaran CD, Bottalico P, et al. Toward a Consensus Description of Vocal Effort, Vocal Load, Vocal Loading, and Vocal Fatigue. J Speech Lang Hear Res [Internet]. 2020;63(2):509-32. doi: https://doi.org/10.1044/2019_JSLHR-19-00057
25. Švec JG, Popolo PS, Titze IR. Measurement of vocal doses in speech: Experimental procedure and signal processing. Logoped Phoniatr Vocol [Internet]. 2003;28(4):181-92. doi: https://doi.org/10.1080/14015430310018892
26. Titze IR, Švec JG, Popolo PS. Vocal Dose Measures: Quantifying Accumulated Vibration Exposure in Vocal Fold Tissues. J Speech Lang Hear Res [Internet]. 2003;46(4):919-32. doi: https://doi.org/10.1044/1092-4388(2003/072)
27. Titze IR, Hunter EJ. Comparison of Vocal Vibration-Dose Measures for Potential-Damage Risk Criteria. J Speech Lang Hear Res [Internet]. 2015;58(5):1425-39. doi: https://doi.org/10.1044/2015_JSLHR-S-13-0128
28. Assad JP, Gama ACC, Santos JN, Castro Magalhães M. The Effects of Amplification on Vocal Dose in Teachers with Dysphonia. J Voice [Internet]. 2019;33(1):73-9. doi: https://doi.org/10.1016/j.jvoice.2017.09.011
29. Morrow SL, Connor NP. Voice Amplification as a Means of Reducing Vocal Load for Elementary Music Teachers. J Voice [Internet]. 2011;25(4):441-6. doi: https://doi.org/10.1016/j.jvoice.2010.04.003
30. Zabret M, Hočevar Boltežar I, Šereg Bahar M. The Importance of The Occupational Vocal Load for The Occurence and Treatment of Organic Voice Disorders. Slovenian Journal of Public Health. Sciendo [Internet]. 2018;57(1):17-24. doi: https://doi.org/10.2478/sjph-2018-0003
31. Alvarez Cáceres R. Ensayos clínicos: diseño, análisis e interpretación. 1st ed. Madrid: Ediciones Diaz de Santos; 2005. 197 p.
32. Atará-Piraquive AP, Herrera-Guzmán CL, Hernández-Contreras JR, Rincón-Pinilla MP, Peña-Campagnoli AT, Florez-Lancheros GP, et al. Effect of a Workplace Vocal Health Promotion Program and Working Conditions on Voice Functioning of College Professors. J Voice [Internet]. 2021;37(6):886-96. doi: https://doi.org/10.1016/j.jvoice.2021.05.016
33. Hunter EJ. Vocal Dose Measures: General Rationale, Traditional Methods and Recent Advances. In I International Conference on Occupational Voice [Internet]. 2016 Sep 16-18; Bogotá, Colombia: Asociación Colombiana de Fonoaudiología (Asofono); 2016. 5 p. Available from: https://www.researchgate.net/publication/311192575_Vocal_Dose_Measures_General_Rationale_Traditional_Methods_and_Recent_Advances
34. Bottalico P, Ipsaro Passione I, Astolfi A, Carullo A, Hunter EJ. Accuracy of the quantities measured by four vocal dosimeters and its uncertainty. J Acoust Soc Am [Internet]. 2018;143(3):1591-602. doi: https://doi.org/10.1121/1.5027816
35. Carullo A, Vallan A, Astolfi A, Pavese L, Puglisi GE. Validation of calibration procedures and uncertainty estimation of contact-microphone based vocal analyzers. Measurement [Internet]. 2015;74:130-42. doi: https://doi.org/10.1016/j.measurement.2015.07.011
36. Costello E. Opening up to open source: looking at how Moodle was adopted in higher education. Open Learning: The Journal of Open, Distance and e-Learning [Internet]. 2013;28(3):187-200. doi: https://doi.org/10.1080/02680513.2013.856289
37. Roy N, Weinrich B, Gray SD, Tanner K, Toledo SW, Dove H, et al. Voice Amplification Versus Vocal Hygiene Instruction for Teachers with Voice Disorders: A Treatment Outcomes Study. J Speech Lang Hear Res [Internet]. 2002;45(4):625-38. doi: https://doi.org/10.1044/1092-4388(2002/050)
38. Timmermans B, Coveliers Y, Wuyts FL, Van Looy L. Voice Training in Teacher Education: The Effect of Adding an Individualized Microteaching Session of 30 Minutes to the Regular 6-Hour Voice Training Program. J Voice [Internet]. 2012;26(5):669.E1-669.E9. doi: https://doi.org/10.1016/j.jvoice.2011.03.001
39. Roy N, Gray SD, Simon M, Dove H, Corbin-Lewis K, Stemple JC. An evaluation of the effects of two treatment approaches for teachers with voice disorders: a prospective randomized clinical trial. J Speech Lang Hear Res [Internet]. 2001;44(2):286-96. doi: https://doi.org/10.1044/1092-4388(2001/023)
40. Pizolato RA, Rehder MIBC, Meneghim MC, Ambrosano GMB, Mialhe FL, Pereira AC. Impact on quality of life in teachers after educational actions for prevention of voice disorders: a longitudinal study. Health Qual Life Outcomes [Internet]. 2013;11:28. doi: https://doi.org/10.1186/1477-7525-11-28
41. Timmermans B, Coveliers Y, Meeus W, Vandenabeele F, Van Looy L, Wuyts F. The Effect of a Short Voice Training Program in Future Teachers. J Voice [Internet]. 2011;25(4):e191-8. doi: https://doi.org/10.1016/j.jvoice.2010.04.005
42. Roy N, Weinrich B, Gray SD, Tanner K, Stemple JC, Sapienza CM. Three Treatments for Teachers with Voice Disorders: A Randomized Clinical Trial. J Speech Lang Hear Res [Internet]. 2003;46(3):670-88. doi: https://doi.org/10.1044/1092-4388(2003/053)
43. Oliveira Bastos PRH, Hermes EC. Effectiveness of the Teacher’s Vocal Health Program (TVHP) in the Municipal Education Network of Campo Grande, MS. J Voice [Internet]. 2018;32(6):681-8. doi: https://doi.org/10.1016/j.jvoice.2017.08.029
44. Rantala L, Sala E, Kankare E. Teachers’ Working Postures and Their Effects on the Voice. Folia Phoniatr Logop [Internet]. 2018;70(1):24-36. doi: https://doi.org/10.1159/000487593
45. Plevin R. Take control of the noisy class. From chaos to calm in 15 seconds. 1st ed. Carmarthen: Crown House Publishing; 2016. 255 p.
46. Wilson Arboleda BM, Frederick AL. Considerations for Maintenance of Postural Alignment for Voice Production. J Voice [Internet]. 2008;22(1):90-9. doi: https://doi.org/10.1016/j.jvoice.2006.08.001
47. Saatweber M. How to Help Teachers’ Voices. Folia Phoniatr Logop [Internet]. 2009;60(6):288-90. doi: https://doi.org/10.1159/000170077
48. Hackworth RS. The effect of vocal hygiene and behavior modification instruction on the self-reported vocal health habits of public school music teachers. International Journal of Music Education [Internet]. 2007;25(1):20-8. doi: https://doi.org/10.1177/0255761407074889
49. Roy N. Optimal dose-response relationships in voice therapy. Int J Speech Lang Pathol [Internet]. 2012;14(5):419-23. doi: https://doi.org/10.3109/17549507.2012.686119
50. Bottalico P, Astolfi A. Investigations into vocal doses and parameters pertaining to primary school teachers in classrooms. J Acoust Soc Am [Internet]. 2012;131(4):2817-27. doi: https://doi.org/10.1121/1.3689549
51. Gaskill CS, O’Brien SG, Tinter SR. The effect of voice amplification on occupational vocal dose in elementary school teachers. J Voice [Internet]. 2012;26(5):667.E19-27. doi: https://doi.org/10.1016/j.jvoice.2011.10.010
52. Atará-Piraquive AP, Forero-Suárez LL, Cárdenas-Martinez JF, Cantor-Cutiva LC. Effect of an online Workplace Vocal Health and Low Stress Levels Promotion Program implemented in a Colombian university during COVID-19 pandemic. CoDAS. 2023;35(6):e20220052. doi: https://doi.org/10.1590/2317-1782/20232022052
53. Cantor-Cutiva LC, Cantor-Cutiva AM. Impact of a Three-Week Workplace Vocal Health Promotion Program on a Teacher and Students’ Voice Parameters. Rev Investig Innov Cienc Salud [Internet]. 2023;5(2):3-23. doi: https://doi.org/10.46634/riics.180
54. Grillo EU. An Online Telepractice Model for the Prevention of Voice Disorders in Vocally Healthy Student Teachers Evaluated by a Smartphone Application. Perspect ASHA Spec Interest Groups [Internet]. 2017;2(3):63-78. doi: https://doi.org/10.1044/persp2.SIG3.63
55. Atará-Piraquive AP, Rute Sanabria BO, Cantor-Cutiva LC. Productivity costs associated to voice symptoms, low sleep quality, and stress among college professors during homeworking in times of COVID-19 Pandemic. Rev Investig Innov Cienc Salud [Internet]. 2022;4(1):4-15. doi: https://doi.org/10.46634/riics.131
56. Karjalainen S, Sahlén B, Falck A, Brännström J, Lyberg-Åhlander V. Implementation and evaluation of a teacher intervention program on classroom communication. Logoped Phoniatr Vocol [Internet]. 2020;45(3):110-22. doi: https://doi.org/10.1080/14015439.2019.1595131
57. Mello MCMBD, Cantor-Cutiva LC, Ferreira LP. Panorama de tres países latinoamericanos en problemas de voz relacionados con condiciones de trabajo. CoDAS [Internet]. 2021;33(5):e20200304. doi: https://doi.org/10.1590/2317-1782/20202020304
58. Eastman SE, Ghasemzadeh H, Van Stan J, Hillman RE, Mehta DD. Quantifying the Occupational Voice Use of Teachers. Perspect ASHA Spec Interest Groups [Internet]. 2023;8(6):1363-79. doi: https://doi.org/10.1044/2023_PERSP-23-00084