Speech-Language Therapist Staffing for the Rehabilitation of Adult and Paediatric In/Outpatients in Chilean Public Hospitals
Dotación fonoaudiológica para la rehabilitación de pacientes adultos y pediátricos en hospitales públicos chilenos
Felipe Gonzalo Rosales Lillo , Patricia Castro Abarca, Antonia Villalón Barrionuevo, Haranni Antonella Aguilera Soto, Teresita Bravo Andrade
Abstract
Introduction. Speech and language therapists are key in health teams; health institutions must have enough staff for quality care.
Objective. To determine the professional provision of speech and language therapy staffing required for in-and-outpatient care of adult and paediatric patients in public hospitals of the Chilean healthcare network.
Method. An observational, descriptive, cross-sectional study was carried out, which included clinical beds of Chilean public hospitals. The calculation was performed according to the Chilean Ministry of Health guidance for estimating the rehabilitation human resources required for in-and-outpatient care, according to the number and type of clinical beds (basic, medium and critical care) available in each public health institutions.
Results. 189 hospitals were included, with 23,677 clinical beds analysed. 81% and 19% of them were for adult and paediatric patient care respectively. 28,950 hours per week of speech and language therapy staffing in public hospitals for in-and-outpatient care is required: 85% for adult patients and 15% for paediatric ones. The Magallanes and Ñuble Regions require the highest percentage of hours -92 and 91%, respectively- for adult patients. The Tarapacá, Metropolitana, and Aysén regions need 18% of hours for paediatric patients. The Metropolitana Region needs almost 35% of the total national hours, followed by Biobío (10.29%) and Valparaíso (9.87%) regions.
Conclusion. Hospitals should review these results to ensure a correct planning of professionals, and consider the proposal for non-working days for the care of hospitalised patients, to optimise their clinical results and quality of life, and the management results of each centre. It is necessary to continue generating evidence in favour of patient care, resource optimisation, and the well-being of clinical professionals.
Keywords
Speech-language pathology; health-planning guidelines; health facilities; hospital administration; Chile.
Resumen
Introducción. Los fonoaudiólogos son clave en los equipos de salud; las instituciones de salud deben contar con personal suficiente para una atención de calidad.
Objetivo. Determinar la dotación profesional de fonoaudiología requerida para la atención abierta y cerrada de pacientes adultos y pediátricos en hospitales públicos de la red asistencial chilena.
Método. Estudio observacional, descriptivo, transversal, que incluyó camas de hospitales públicos chilenos. El cálculo se realizó de acuerdo a la guía del Ministerio de Salud de Chile para la estimación de los recursos humanos en rehabilitación requeridos para atención hospitalaria y ambulatoria, según el número y tipo de camas clínicas (básicas, medias y críticas) disponibles en cada institución de salud pública.
Resultados. 189 hospitales fueron analizados, con 23.677 camas clínicas, 81% para la atención de pacientes adultos y 19% para pacientes pediátricos. A nivel nacional, se requieren 28.950 horas semanales de fonoaudiología en los hospitales públicos para la atención abierta y cerrada: 85% para pacientes adultos y 15% para pediátricos. Las regiones de Magallanes y Ñuble concentran el mayor porcentaje de requerimiento para pacientes adultos (92 y 91%). Las regiones de Tarapacá, Metropolitana y Aysén, por su parte, requieren 18% para pacientes pediátricos (18%). La Región Metropolitana contempla cerca del 35% del requerimiento nacional, seguido del Biobío (10,29%) y Valparaíso (9,87%).
Conclusión. Se sugiere que cada hospital revise estos resultados para garantizar una planificación adecuada de profesionales. También se debe considerar la propuesta para días inhábiles para atención de pacientes hospitalizados, y así optimizar los resultados clínicos, los aspectos de calidad de vida y de gestión institucional. Es necesario continuar generando evidencia a favor de la atención, la optimización de recursos y el bienestar de los profesionales clínicos.
Palabras clave
Fonoaudiología; directrices para la planificación en salud; instituciones de salud; administración hospitalaria; Chile.
Introduction
The role of speech and language therapists (SLTs) in health teams has been widely valued internationally, supported by public policies and studies. Their importance is underlined in the evaluation and management of communication and swallowing of patients, the education of health professionals, patients, family members, and caregivers, as well as their active participation in interdisciplinary teams [1-8]. The function of SLTs is considered essential to offer quality care for patients, presenting a timely diagnosis, providing effective rehabilitation and improving their clinical results [9]. Guaranteeing early and intensive rehabilitation is key to improve the patient's discharge conditions, reducing the length of hospital stay, decreasing the risk of disability, and reducing the degree of dependency [10]. A critical area in which SLTs play a crucial role in the health context is in the management of patients suffering from dysphagia, which can have serious clinical repercussions on public health. The literature indicates that dysphagia significantly increases the risk of hospital readmissions, the development of serious secondary complications such as aspiration pneumonia, malnutrition, dehydration, sarcopenia, and, ultimately, death [11-18]. In critical care patients, dysphagia has been associated with an increased mortality rate of 9.2% [19]. In hospitalised patients, dysphagia rises the care costs because of additional interventions, the use of clinical supplies and inputs, and the increase of drug prescriptions [20]. It has been reported that older patients with hip and/or femur fractures accompanied by dysphagia have an average hospital stay more than twice as long as those without dysphagia. Additionally, these patients have a mortality rate four times higher and a rate of aspiration pneumonia 14 times higher. This would imply an additional expenditure to health systems of 66% [12]. Evidence suggests that prevention strategies for dysphagia-related complications in healthcare institutions (HI) are cost-effective [21,22]. Regarding communication disorders, hospitalised patients who fail to express themselves effectively are three times more likely to experience preventable adverse events, including the risk of falls [23].
The shortage of SLTs in HI increases care costs for health centres, mainly due to the lack of timely diagnosis and effective treatment for patients with dysphagia [20]. This situation constitutes a public health problem since it directly impacts the clinical results of patients and deteriorates their quality of life (QoL). In this sense, the comprehensive and specialised approach provided by SLTs is presented as an effective strategy to mitigate the risks associated with these disorders, as well as to optimise clinical results and resource efficiency. HI must have sufficient clinical staff to guarantee quality care. Internationally, there is no single guideline on the most appropriate approach to estimate the SLTs needed in HIs. There are different proposals for ratios based on hospital clinical beds (CBs), ranging from .025 to 2.000 full-time SLTs (FTSLTs) for every 10 CBs [7,24-30]. The Intensive Care Society of the United Kingdom has indicated that the speech and language therapy staffing (SLT-S) required will depend on the complexity and services that each centre provides individually [26]. Additionally, the National Health Service of the United Kingdom specifies that, to guarantee patient care, it is desirable to have service of speech and language therapy (SLT) in HIs seven days a week [31]. The Chilean Ministry of Health (MINSAL) established a rehabilitation guideline to determine the human resources for rehabilitation required in hospitals of the healthcare network, including SLTs. The formula considers the number and type of CBs available [10]. This guideline was based on two international references, a position paper [32] and a literature review [33]. With the ratios indicated in both publications, the MINSAL made an internal adjustment to the classification. The formula is applied to both in-and-outpatient care (IOC). Additionally, the formula suggests that, given the greater proportion of hospitalised older adults who present a higher degree of dependency and need for support, an adjustment should be applied to the basic care CBs. Specifically, 70% of the basic care CBs should be considered as medium care CBs.
It is important to consider that the proposed result corresponds to the SLT-S for patients care on working days, which does not include the SLT-S hours for audiology services. Table 1 shows the formula for calculating the SLT-S proposed by the MINSAL.
Table 1. Formula for calculating the professional provision of speech and language therapy based on the number and types of hospital clinical beds, proposed by the Ministry of Health of Chile in 2019.
| Types of clinical bed | Formula | ||||
|---|---|---|---|---|---|
| -Basic care clinical beds (BCBs) | (Number of BCBs | / | 10) | x | .06 |
| -Medium care clinical beds (MCBs) | (Number of MCBs | / | 10) | x | .23 |
| -Paediatric critic care clinical beds (PCCBs) | (Number of PCCBs | / | 6) | x | .46 |
| -Adult critic care clinical beds (ACCBs) | (Number of ACCBs) | / | 6) | x | .23 |
This study seeks to detail the SLT-S required in healthcare institutions in Chile during working days, which may support decision-making by health managers and clinicians in different public hospitals. In addition, it is presented an alternative of SLT-S hours required during non-working days to guarantee continuity of SLT care for adult and paediatric patients hospitalised seven days a week. The research question of this study was: What is the SLT-S required for IOC of adult and paediatric patients in public hospitals of the Chilean healthcare network? The objective of this project was to determine the professional provision of SLT-S required for in-and-outpatient care of adult and paediatric patients in public hospitals of the Chilean healthcare network.
Method
Design
Observational, descriptive, cross-sectional study.
Population and sample
Public hospitals of the Chilean healthcare network, which attend adult and paediatric patients. The unit of analysis corresponds to each CBs in the healthcare network, according to their type.
Inclusion criteria
Chilean public hospitals for the care of adult and paediatric patients, including the care of neonatal patients.
Exclusion criteria
CBs for attending obstetric, gynaecologic and psychiatric patients.
Variables
Numerical data of basic care, medium care and critical care CBs in both adults and paediatrics patients were considered. Additionally, categorical data of hospitals and regions of the country were considered.
Instruments
Microsoft Excel 2016, MINSAL guideline document for calculating professional staff [10] (see Table 1 that shows the formula for calculating the SLT-S proposed by the MINSAL), public information on the number and type of CBs in Chilean hospitals available on the website of the Department of Statistics and Health Information (Departamento de Estadísticas e Información de Salud) of MINSAL [34]. The use of artificial intelligence-assisted technology (ChatGPT) was implemented to review and improve the scientific writing of the manuscript.
Procedures
First, the CBs data from the MINSAL website [34] were transferred to a Microsoft Excel 2016 database, where non-useful data were eliminated, comparing the number of CBs by type for each hospital and by region. The type of CBs according to the MINSAL formula [10] are basic care clinical beds (BCBs), medium care clinical beds (MCBs), adult critical care clinical beds (ACCBs) and paediatric critical care clinical beds (PCCB). Additionally, based on the type of bed per hospital, the BCB and MCB were grouped into paediatrics and adult beds (PBCBs, ABCBs, PMCBs and AMCBs). Subsequently, the calculation was performed by each hospital to determine the number of hours of SLT-S required weekly. Finally, a proposal was made for the care of hospitalised patients on non-working days to provide continuity of care seven days a week.
Data analysis
Descriptive statistics were applied to numerical and categorical variables. Due to the nature of the study, statistical analysis was not required.
Ethics considerations
This project, as it did not involve the participation of subjects, but rather exclusively the analysis of public data, did not require ethical approval by a research ethics committee for its implementation.
Results
After applying inclusion and exclusion criteria, 189 hospitals from the healthcare network were selected for analysis.
CCH
A total of 23,677 clinical beds were identified in Chilean public hospitals, of which approximately 81% (n = 19,317) were for the care of adult patients, while approximately 19% (n = 4,360) for paediatric patients. The proportion of basic care, medium care, and critical paediatric care CBs were similar, with 1,438, 1,436 and 1,486 units respectively. 35% of the CBs for the care of adult patients corresponded to basic care CBs (n = 6,782), 51% to medium care CBs (n = 9,747), and 14% to critical care CBs (n = 2,788). The distribution of adult and paediatric care CBs by type, by region and at the national level is detailed in Table 2. The Supplemental material specifies the number of CBs by HI.
Table 2. Distribution of adult and paediatric hospital clinical beds by type, by region, and at national level.
| Region | Adult basic care CBsa | Paediatric basic care CBsa | Adult medium care CBsa | Paediatric medium care CBsa | Adult critic care CBsa | Paediatric critic care CBsa | Total adult care CBa | Total paediatric care CBa | Total CBa |
|---|---|---|---|---|---|---|---|---|---|
| Arica y Parinacota | 30 | 3 | 175 | 18 | 36 | 20 | 241 | 41 | 282 |
| Tarapacá | 51 | 29 | 186 | 5 | 42 | 42 | 279 | 76 | 355 |
| Antofagasta | 137 | 54 | 447 | 70 | 100 | 45 | 684 | 169 | 853 |
| Atacama | 117 | 44 | 176 | 13 | 40 | 20 | 333 | 77 | 410 |
| Coquimbo | 105 | 56 | 518 | 78 | 135 | 54 | 758 | 188 | 946 |
| Valparaíso | 873 | 128 | 940 | 142 | 253 | 113 | 2,066 | 383 | 2,449 |
| Metropolitana | 1,898 | 292 | 3,054 | 601 | 1,123 | 686 | 6,075 | 1,579 | 7,654 |
| O'Higgins | 165 | 25 | 572 | 51 | 144 | 83 | 881 | 159 | 1,040 |
| Maule | 605 | 146 | 485 | 72 | 162 | 72 | 1,252 | 290 | 1,542 |
| Ñuble | 396 | 86 | 188 | 3 | 72 | 29 | 656 | 118 | 774 |
| Biobío | 857 | 240 | 1,120 | 123 | 233 | 117 | 2,210 | 480 | 2,690 |
| Araucanía | 541 | 126 | 861 | 139 | 176 | 81 | 1,578 | 346 | 1,924 |
| Los Ríos | 345 | 102 | 297 | 20 | 54 | 28 | 696 | 150 | 846 |
| Los Lagos | 404 | 67 | 572 | 83 | 159 | 69 | 1,135 | 219 | 1,354 |
| Aysén | 55 | 17 | 85 | 18 | 17 | 11 | 157 | 46 | 203 |
| Magallanes | 203 | 23 | 71 | 0 | 42 | 16 | 316 | 39 | 355 |
| Total country | 6,782 | 1,438 | 9,747 | 1,436 | 2,788 | 1,486 | 19,317 | 4,360 | 23,677 |
Note. a: Clinical beds
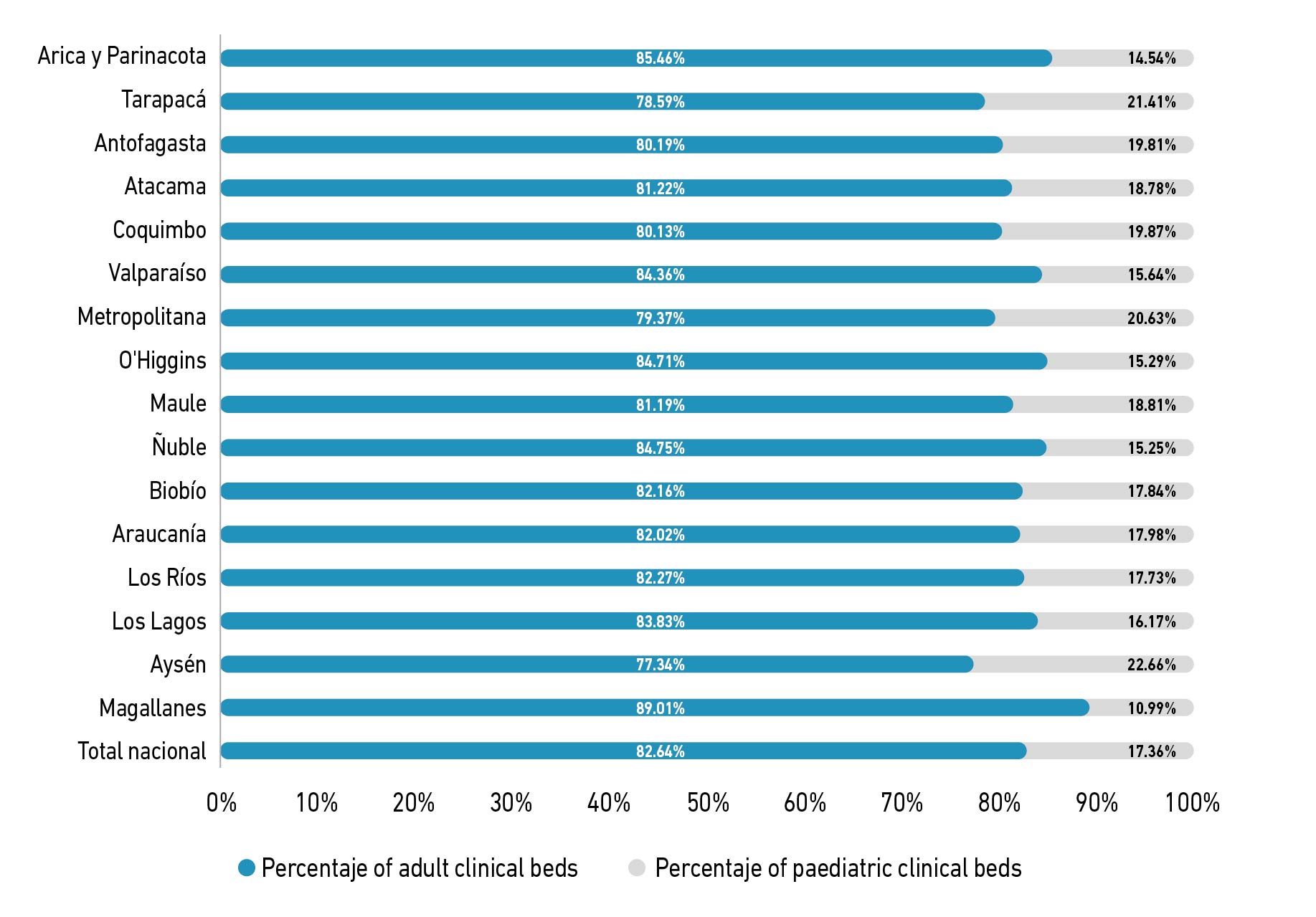
When analysing the CBs by region and patient group (adult or paediatric), it can be noticed that in all regions predominated adult CBs with percentages close to 80%. The Aysén Region had the highest percentage of paediatric CBs at the national level (22.66%), whilst the Magallanes Region had the lowest proportion (10.99%). Figure 1 shows the percentage of adult and paediatric care CBs by region and at the national level.
Figure 1. Percentage of adult and pediatric hospital clinical beds by region and at national level.
Weekly SLT-S hours required
After applying the MINSAL formula [10], it was found that at a national level, 28,950 weekly hours of SLT-S are required in public hospitals. Of this, 24,610 hours are required for the IOC of adult patients (85%), while the IOC of paediatric patients required 4,339 (15%). Magallanes and Ñuble regions concentrate the highest percentage of hours for the IOC of adult patients, with 92 and 91%, respectively. Tarapacá, Metropolitana and Aysén regions, on the other hand, for the IOC of paediatric patients (18% each). Table 3 details the approximate weekly hours of SLT required for the IOC of adult and paediatric patients by region and at a national level. The Metropolitana Region accounts for about 35% of the national requirement, followed by the Biobío Region (10.29%), and the Valparaíso Region (9.87%). Supplemental material details the weekly hours of SLT-S required by HI.
Table 3. Approximate weekly hours of speech and language therapy required for in-and-outpatient care of adult and paediatric patients by region and at the national level.
| Region | Hours for adult patient care | Percentage of hours for adult patient care | Hours for paediatric patient care | Percentage of hours for paediatric patient care | Total of hours for patient care |
|---|---|---|---|---|---|
| Arica y Parinacota | 322 | 86% | 53 | 14% | 375 |
| Tarapacá | 370 | 82% | 84 | 18% | 454 |
| Antofagasta | 898 | 85% | 161 | 15% | 1,059 |
| Atacama | 405 | 87% | 59 | 13% | 464 |
| Coquimbo | 1,062 | 85% | 185 | 15% | 1,247 |
| Valparaíso | 2,492 | 87% | 368 | 13% | 2,860 |
| Metropolitana | 8,374 | 82% | 1,842 | 18% | 10,216 |
| O'Higgins | 1,195 | 86% | 198 | 14% | 1,393 |
| Maule | 1,514 | 87% | 233 | 13% | 1,747 |
| Ñuble | 745 | 91% | 75 | 9% | 820 |
| Biobío | 2,594 | 87% | 385 | 13% | 2,980 |
| Araucanía | 1,891 | 86% | 311 | 14% | 2,202 |
| Los Ríos | 754 | 89% | 94 | 11% | 849 |
| Los Lagos | 1,433 | 87% | 218 | 13% | 1,651 |
| Aysén | 187 | 82% | 41 | 18% | 228 |
| Magallanes | 373 | 92% | 33 | 8% | 406 |
| Total country | 24,610 | 85% | 4,339 | 15% | 28,950 |
Proposal for a SLT-S for inpatient care during non-working days
To ensure the continuous care of hospitalised patients seven days a week, Supplemental material details the daily hours to be considered for each non-working day for each HI. This estimate was obtained by dividing the weekly hours of the formula into five, in order to obtain an average daily value. It is necessary to take into consideration that this result includes hours for both in- and outpatient care (IOC). In order to determine the exclusive hours required on non-working days for inpatient care, each hospital must consider the total daily hours of staffing for outpatient care. These hours must be subtracted from the daily total proposed in Supplemental material. Additionally, the non-clinical daily hours carried out by inpatient care professionals on working days, associated with the speech therapy activities indicated in the MINSAL guidelines [10], must be determined, these being team meetings, administrative meetings, knowledge development and self-care, and training or extension activities. Finally, it is suggested to add sufficient time for the SLTs to the result to ensure the participation on the ward multidisciplinary team visits.
Discussion
The objective of this research was to determine the professional provision of SLT-S required for in-and-outpatient care of adult and paediatric patients in public hospitals of the Chilean healthcare network.
The role of SLTs in health is widely documented [1-8], where their function as a key to providing quality care to users is also highlighted [9]. In addition, there have been reported adverse effects for patients associated with communication and swallowing disorders [11-18], which include increased risk of falls [23], and even death [19]. In addition, extra expenditure for HI that must provide extra resources, including supplies, drugs, use of hospital bed-days, human resources, among others, which generates important repercussions as it is a public health problem [20-22]. The lack of SLTs in HI delays the timely diagnosis of communication and swallowing disorders, as well as interdisciplinary management. As a consequence, the start of timely rehabilitation is postponed, increasing the morbidity of those who require care. This situation generates a reduction in the QoL of patients in their aspects of mental and social health status, functionality, physical and general well-being, and satisfaction. It also affects the immediate family, mainly family members and/or caregivers. HI that do not have an optimal SLT-S widen the inequality in health regarding adequate access to clinical care. After hospital discharge, a significant percentage of patients need to continue their rehabilitation process on an outpatient basis. Inopportune access to care during the hospitalisation period causes patients to have a longer period of disability and reduced functionality upon discharge, which in the long term can cause a greater clinical and QoL impact. It also has economic consequences for health system. Delaying the recovery of functionality for those who are of working age prolongs their return to work. Therefore, it is essential that hospitals can carry out an adequate survey of their local contexts, determining their current SLT-S and its distribution for IOC.
The MINSAL declares that human resources in hospitals are insufficient to meet the care requirements, in which it is necessary to reduce the gap in rehabilitation professionals [10]. Having sufficient clinical staff is key to guarantee quality care and reduce negative impacts. To this end, multiple SLT-S proposals have been raised internationally, where there is no single ratio guideline for calculation [7,24-30]. These ratios are between .025 and 2.000 FTSLTs for every 10 CBs for inpatient care, according to different factors, including number of beds and pathology of patients. For the national case [10], this ratio covers a range between .07 and .76 FTSLTs for every 10 CBs, according to number and type of CB, for IOC. It is important to mention at this point, that the MINSAL guidance considerer a greater ratio for physiotherapist and occupational therapists in comparison to SLTs. Psychologists and social workers are just taken into account for critical care settings. The total number of beds determines the number of full-time rehabilitation physicians required: one physician is needed for every 200 clinical beds, with an additional physician required for every 100 beds beyond that [10]. It is important to consider that a full-time work schedule in Chile for the public system establishes a total of 44 hours per week [35].
According to international SLT-S ratios versus the national one mentioned previously, three main differences can be highlighted. The minimum ratio of the national formula is higher than that of the available evidence. This is because international literature has included specific pathologies where speech therapy care is less, which is why the ratio is reduced [24,30]. In the case of the maximum ratio, at an international level for both critical and neurological patients, it is close to double the national ratio [24,27,30]. This guarantees more targeted and repeated care for users who require it. Finally, in the case of Chile, the results of professional staffing must be distributed to guarantee speech therapy, so the actual number of hours exclusively for hospitalised users would be lower.
Regarding the continuity of care, the MINSAL formula establishes its provision during working days, unlike international recommendations that indicate that it is desirable to have speech therapists seven days a week [31]. Regarding the activities of SLTs according to MINSAL guidelines, the following stand out: initial and intermediate evaluation (40 minutes), individual (30 minutes) and group (60-120 minutes) rehabilitation sessions, team meetings (60-120 minutes per week), administrative meetings (60 minutes per week), knowledge development and self-care (60 minutes per week), and outreach and training (unspecified) [10]. Considering a 44-hour workweek, it can be concluded that for non-clinical activities (excluding outreach and training), adding also the 30-minute lunch break per day (150 minutes per week), FTSLTs should allocate around 6.5 hours per week for these tasks [35]. Thus, the number of hours for work with patients would be 37.5 hours per week, and could be even less. One point not specified in the guideline is the daily time reserved for ward visits with the multidisciplinary team, in the case of inpatient care, as it is mentioned by the literature as key [1-8]. It would be optimal if the national authorities could carry out a review of the previous points, to consider a re-evaluation of the MINSAL guideline, including the continuity of care seven days a week. In addition, clinical services can be determined according to the type of users and their pathologies [24-30].
The results of the required SLT-S according to the MINSAL formula [10] must be reviewed in detail by each Chilean hospital, so that clinical SLTs together with health managers can carry out an adequate planning of human resources for IOC. For those institutions with SLT-S below the number of hours calculated, they are invited to take the necessary steps to achieve a shortening of the professional gap. It is suggested that each hospital carries out an in-depth analysis of the professional requirement, since the need for SLTs could be even greater than estimated in the MINSAL calculation, associated with variables such as the institutional context, patient needs and their complexity, profiles, pathologies, workload, physical resources, available technologies, among others [10,24-30]. It is important to emphasise that audiology services must be planned with additional human resources to the results presented [10].
Additionally, a proposal with an increase in hours for inpatient care during non-working days is presented for review by clinicians and managers, so that health institutions that are in a position to do so can implement a system that guarantees the continuity of care seven days a week (supplementary material). Regardless of the decision and/or capacity of each centre to implement a staffing according to the MINSAL guideline [10] or one that guarantees the continuity of care, it is necessary to respond to the efficient use of resources, optimising the clinical and management results of each centre.
Limitations and recommendations
As a limitation, it should be noted that the MINSAL guideline presents some difficulties for its interpretation. An example of this is the specified details regarding space and material resources for the SLT room for outpatient care, where there is professional calculation data that are difficult to understand due to errors in the information provided. Clarification of this point was requested for its correct definition. This response will be used to make a formal proposal for SLT care for outpatient care during working hours, as well as continuity seven days a week for inpatient care. It is recommended to continue with this line of research, primarily with a study of the professional gap, considering the reported data. Additionally, new proposals that generate sufficient evidence in all the areas that SLTs intervene, namely by speech, language, social and cognitive communication, and swallowing disorders in both adult and paediatric population [36]. This, including clinical outcomes and cost-effectiveness methods, which could optimise the quality of patients’ care that includes the detection of human resource needs and possibly, their shortage. Also, to improve clinical results through constant training and adequate distribution of human resources. Further, to adequately plan professional resources through new, more efficient strategies. Moreover, to generate adjustments to health demands according to the needs of patients and the clinical context. Finally, they should aim to reduce healthcare costs and promote the well-being of SLTs who work in the area.
Conclusions
The professional provision of speech and language therapy required for in-and-outpatient care of adult and paediatric patients in public hospitals of the Chilean healthcare network corresponds to 28,950 hours per week, where 85% are needed for adult patients and 15% for paediatric patients. The Metropolitana Region accounts for approximately 35% of the national requirement, followed by the Biobío Region (10.29%), and the Valparaíso Region (9.87%).
It is mandatory that the requirement be reviewed by each health institution, so that clinical speech and language therapists and the corresponding managers can adequately plan the distribution of the professional resource for in-and-outpatient according to ministerial guidelines (excluding audiology services). This requirement could be higher depending on the features of each centre and the needs of patients.
In order to provide continuity of speech and language therapy care for hospitalised patients on non-working days, therefore providing care seven days a week, a proposal was was developed which must be reviewed by each hospital according to its particular characteristics.
This research provides valuable evidence for health managers, in public and private settings, to develop protocols and guidelines aimed at ensuring the necessary SLT staffing to meet patient needs. By offering concrete data and analysis, it strengthens the foundation for strategic decision-making in healthcare planning, further enhancing the relevance and impact on patient care.
References
1. American Speech-Language-Hearing Association (ASHA) [Internet]. Rockville: ASHA; c2025. Employment settings for SLPs; 2022 [cited 2024 Mar 15]; [about 3 screens]. Available from: Available from: https://www.asha.org/students/employment-settings-for-slps/
2. Cambridge University Hospitals, NHS Foundation Trust (CUH) [Internet]. Cambridge: CUH; c2025. Speech and language therapy; 2019 [cited 2024 Feb 20]; [about 4 screens]. Available from: Available from: https://www.cuh.nhs.uk/addenbrookes-hospital/services/speech-and-language-teams
3. Joubert S [Internet]. Boston: Northeastern University; c2025. Medical speech-language pathology: The SLP’s role in healthcare; 2021 Sep 15 [cited 2024 Jul 12]; [about 8 screens]. Available from: Available from: https://graduate.northeastern.edu/resources/medical-speech-language-pathology/
4. Mayo Clinic College of Medicine and Science [Internet]. Rochester: Mayo Clinic; c2025. Medical speech-language pathologist; 2022 [cited 2024 May 15] [about 9 screens]. Available from: Available from: https://college.mayo.edu/academics/explore-health-care-careers/careers-a-z/medical-speech-language-pathologist/
5. McGrath BA, Wallace S. The UK National Tracheostomy Safety Project and the role of speech and language therapists. Curr Opin Otolaryngol Head Neck Surg [Internet]. 2014;22(3):181-7. doi: https://doi.org/10.1097/MOO.0000000000000046
6. McRae J, Montgomery E, Garstang Z, Cleary E. The role of speech and language therapists in the intensive care unit. J Intensive Care Soc [Internet]. 2020;21(4):344-8. doi: https://doi.org/10.1177/1751143719875687
7. Royal College of Speech & Language Therapists (RCSLT). Position statement: Speech and language therapists working in adult and paediatric critical care units [Internet]. 2019 [cited 2024 Jan 23]. Available from: Available from: https://www.rcslt.org/-/media/docs/clinical-guidance/rcslt-position-statement-critical-care.pdf
8. Royal College of Speech and Language Therapists (RCSLT) [Internet]. London: RCSLT; c2025. What can you expect from speech and language therapy in critical care?; 2022 [cited 2024 Jan 23] [about 5 screens]. Available from: Available from: https://www.rcslt.org/speech-and-language-therapy/clinical-information/critical-care/
9. Needham DM. Mobilizing patients in the intensive care unit: improving neuromuscular weakness and physical function. JAMA. 2008 Oct 8;300(14):1685-90. doi: https://doi.org/10.1001/jama.300.14.1685
10. Unidad de Rehabilitación, Departamento de Gestión de Procesos Asistenciales Integrados, División de Gestión de Redes Asistenciales. Modelo de Gestión Red de Rehabilitación [Internet]. Santiago: Ministerio de Salud de Chile; 2019 [cited 2024 May 27]. 84 p. Available from: Available from: https://web.archive.org/web/20200623125747/https://www.araucaniasur.cl/wp-content/uploads/2019/06/MODELO-DE-GESTION-RED-DE-REHABILITACION.pdf
11. Alcalde S, Rodríguez R, Ricote M. Guía de disfagia: Manejo de la disfagia en atención primaria [Internet]. Madrid: Sociedad Española de Médicos de Atención Primaria (Semergen); 2020. 74 p. Available from: https://semergen.es/files/docs/grupos/digestivo/manejo-disfagia-ap.pdf
12. Allen J, Greene M, Sabido I, Stretton M, Miles A. Economic costs of dysphagia among hospitalised patients. Laryngoscope [Internet]. 2019;130(4):974-9. doi: https://doi.org/10.1002/lary.28194
13. Altman KW, Yu GP, Schaefer SD. Consequence of dysphagia in the hospitalised patient: impact on prognosis and hospital resources. Arch Otolaryngol Head Neck Surg [Internet]. 2010;136(8):784-9. doi: https://doi.org/10.1001/archoto.2010.129
14. Attrill S, White S, Murray J, Hammond S, Doeltgen S. Impact of oropharyngeal dysphagia on healthcare cost and length of stay in hospital: a systematic review. BMC Health Serv Res [Internet]. 2018;18(1):594. doi: https://doi.org/10.1186/s12913-018-3376-3
15. Cohen DL, Roffe C, Beavan J, Blackett B, Fairfield CA, Hamdy S, et al. Post-stroke dysphagia: a review and design considerations for future trials. Int J Stroke [Internet]. 2016;11(4):399-411. doi: https://doi.org/10.1177/1747493016639057
16. Dziewas R, Allescher HD, Aroyo I, Bartolome G, Beilenhoff U, Bohlender J, et al. Diagnosis and treatment of neurogenic dysphagia - S1 guideline of the German Society of Neurology. Neurol Res Pract [Internet]. 2021;3(1):23. doi: https://doi.org/10.1186/s42466-021-00122-3
17. Suárez Quesada A, Alvarez Aliaga A, Pupo Jimenez JM, Berdú Saumell J, Hernandez Galano ME. Relación entre los indicadores del estado nutricional y el desarrollo de neumonía asociada al ictus isquémico. Rev Finlay [Internet]. 2020;10(3):231-9. Available from: https://revfinlay.sld.cu/index.php/finlay/article/view/765
18. Warnecke T, Dziewas R, Langmore S. Neurogenic dysphagia. Cham: Springer; 2021. 399 p.
19. Schefold J, Berger D, Zürcher P, Lensch M, Perren A, Jakob SM, et al. Dysphagia in mechanically ventilated ICU patients (DYnAMICS): a prospective observational trial. Crit Care Med [Internet]. 2017;45(12):2061-9. doi: https://doi.org/10.1097/CCM.0000000000002765
20. Duncan S, Gaughey JM, Fallis R, McAuley DF, Walshe M, Blackwood B. Interventions for oropharyngeal dysphagia in acute and critical care: a protocol for a systematic review and meta-analysis. Syst Ver [Internet]. 2019;8(1):283. doi: https://doi.org/10.1186/s13643-019-1196-0
21. Marin S, Ortega O, Serra-Prat M, Valls E, Perez-Cordon L, Clave P. Economic evaluation of clinical, nutritional and rehabilitation interventions on oropharyngeal dysphagia after stroke: a systematic review. Nutrients [Internet]. 2023;15(7):1714. doi: https://doi.org/10.3390/nu15071714
22. Qureshi AI, Suri MFK, Huang W, Akinci Y, Chaudhry MR, Pond DS, et al. Annual direct cost of dysphagia associated with acute ischemic stroke in the United States. J Stroke Cerebrovasc Dis [Internet]. 2022;31(5):106407. doi: https://doi.org/10.1016/j.jstrokecerebrovasdis.2022.106407
23. Cardinal A, Freeman-Sanderson A, Togher L. The speech pathology workforce in intensive care units: results from a national survey. Aust Crit Care [Internet]. 2020;33(3):250-8. doi: https://doi.org/10.1016/j.aucc.2020.02.003
24. Allied Health in Rehabilitation Consultative Committee. Guidelines for Allied Health: Resources required for the provision of quality rehabilitation services. 2007. 16 p.
25. Henley J, Bennett C, Williamson J, Scott I. Standards for Medical Assessment and Planning Units in Public and Private Hospitals: Position Statement of the Internal Medicine Society of Australia and New Zealand [Internet]. Auckland, Brisbane, Perth: IMSANZ; 2006 May [cited 2024 Jan 23]. 21 p. Available from: Available from: https://www.imsanz.org.au/common/Uploaded%20files/IMSANZ%20website%20documents/Standards%20for%20Medical%20Assessment%20and%20Planning%20Units%20in%20Public%20and%20Private%20Hospitals.pdf
26. Intensive Care Society. Guidelines for the provision of intensive care services: The Faculty of Intensive Care Medicine [Internet]. London: The Faculty of Intensive Care Medicine / Intensive Care Society; 2022 Jul [cited 2024 Jan 23]. 216 p. Available from: Available from: https://www.ficm.ac.uk/sites/ficm/files/documents/2022-07/GPICS%20V2.1%20%282%29.pdf
27. McHugh G, Swain A. A comparison between reported therapy staffing levels and the department of health therapy staffing guidelines for stroke rehabilitation: a national survey. BMC Health Serv Res [Internet]. 2014;14:216. doi: https://doi.org/10.1186/1472-6963-14-216
28. Mudge A, Laracy S, Richter K, Denaro C. Controlled trial of multidisciplinary care teams for acutely ill medical inpatients: enhanced multidisciplinary care. Intern Med J [Internet]. 2006;36(9):558-63. doi: https://doi.org/10.1111/j.1445-5994.2006.01135.x
29. National Clinical Programme for Stroke. National Stroke Strategy 2022-2027 [Internet]. Dublin: Royal College of Physicians of Ireland / National Clinical Programme for Stroke; 2022 [cited 2024 May 27]. 88 p. Available from: Available from: https://www.hse.ie/eng/services/publications/clinical-strategy-and-programmes/national-stroke-strategy-2022-2027.pdf
30. The Royal Australasian College of Physicians (RACP), Australasian Faculty of Rehabilitation Medicine (AFRM). Standards for the provision of inpatient adult rehabilitation medicine services in public and private hospitals [Internet]. Sydney: RACP / AFRM; 2019 Feb [cited 2024 May 27]. 19 p. Available from: Available from: https://www.racp.edu.au/docs/default-source/advocacy-library/afrm-standards-for-the-provision-of-inpatient-adult-rehabilitation-medicine-services-in-public-and-private-hospitals.pdf?sfvrsn=4690171a_4
31. National Health Service. Schedule 2 - The Services [Internet]. 2019 [cited 2024 May 27]. Available from: Available from: https://web.archive.org/web/20210130145122/https://www.england.nhs.uk/wp-content/uploads/2019/05/Adult-Critical-Care-Service-Specification-FINAL.pdf
32. Ward AB, Gutenbrunner C, Damjan H, Giustini A, Delarque A. European Union of Medical Specialists (UEMS) section of Physical & Rehabilitation Medicine: a position paper on physical and rehabilitation medicine in acute settings. JRM [Internet]. 2010;42(5):417-24. doi: https://doi.org/10.2340/16501977-0565
33. Cartmill L, Comans TA, Clark MJ, Ash S, Sheppard L. Using staffing ratios for workforce planning: evidence on nine allied health professions. Hum Resour Health [Internet]. 2012;10(2):1-8. doi: https://doi.org/10.1186/1478-4491-10-2
34. Ministerio de Salud de Chile. Dotación de camas hospitalarias de establecimientos pertenecientes al SNSS (públicos) por servicio de salud, establecimiento y área funcional [Internet]. Departamento de Estadísticas e Información de Salud; 2023 [cited 2024 Sep 30]. Available from: Available from: https://repositoriodeis.minsal.cl/ContenidoSitioWeb2020/Estadisticas/DOTACION_CAMAS/Dotaci%C3%B3n%20de%20camas%202010-2023%20Establecimientos%20Pertenecientes%20al%20SNSS.xlsx
35. Ley N° 18.834. Estatuto Administrativo. Texto refundido, coordinado y sistematizado fijado por Decreto con Fuerza de Ley N° 29 de 2004. Diario Oficial 2017 Dec 7. Available from: https://www.dt.gob.cl/portal/1626/articles-117137_galeria_36.pdf
36. American Speech-Language-Hearing Association (ASHA) [Internet]. Rockville: ASHA; c2025. Speech-language pathologists; 2025 [citado 2025 abr 14] [about 4 screens]. Available from: Available from: https://www.asha.org/students/speech-language-pathologists/?srsltid=AfmBOoq-8hQ9aMZ7_lMdpfSSjTidV3ZOfdjpRg-19V_A13ZBs_WLi72r