Occupational Health Conditions Among Healthcare Workers During the COVID-19 Pandemic
Condiciones de la Salud Ocupacional en Trabajadores de la Salud Durante la Pandemia de COVID-19
Teobaldo Ortiz-Ramirez, Christian Soledad Ortiz-Chacha , Jaime Morales-Romero, Nemesio Castillo-Viveros, Esteban Picazzo-Palencia
Abstract
Introduction. The COVID-19 pandemic created a stage of vulnerability for healthcare workers, whose working conditions and health were affected by the increased demand for care of patients infected with the SARS-CoV-2 virus in the hospital setting, altering the occupational health conditions in several areas.
Objective. We aimed to analyze the occupational health conditions of healthcare workers in a secondary care hospital during the first year of the COVID-19 pandemic.
Method. A quantitative, observational, and retrospective study was conducted on a sample of 159 healthcare workers from a secondary care hospital clinic. A 103-item questionnaire with five domains covering sociodemographic, occupational, and health variables, including those related to occupational health, was used. We used univariate analysis to describe the study population, while bivariate analysis for the difference in proportions and multivariate analysis for variable reduction. Data analysis and visualization were performed using the R Studio software, version 4.0.3.
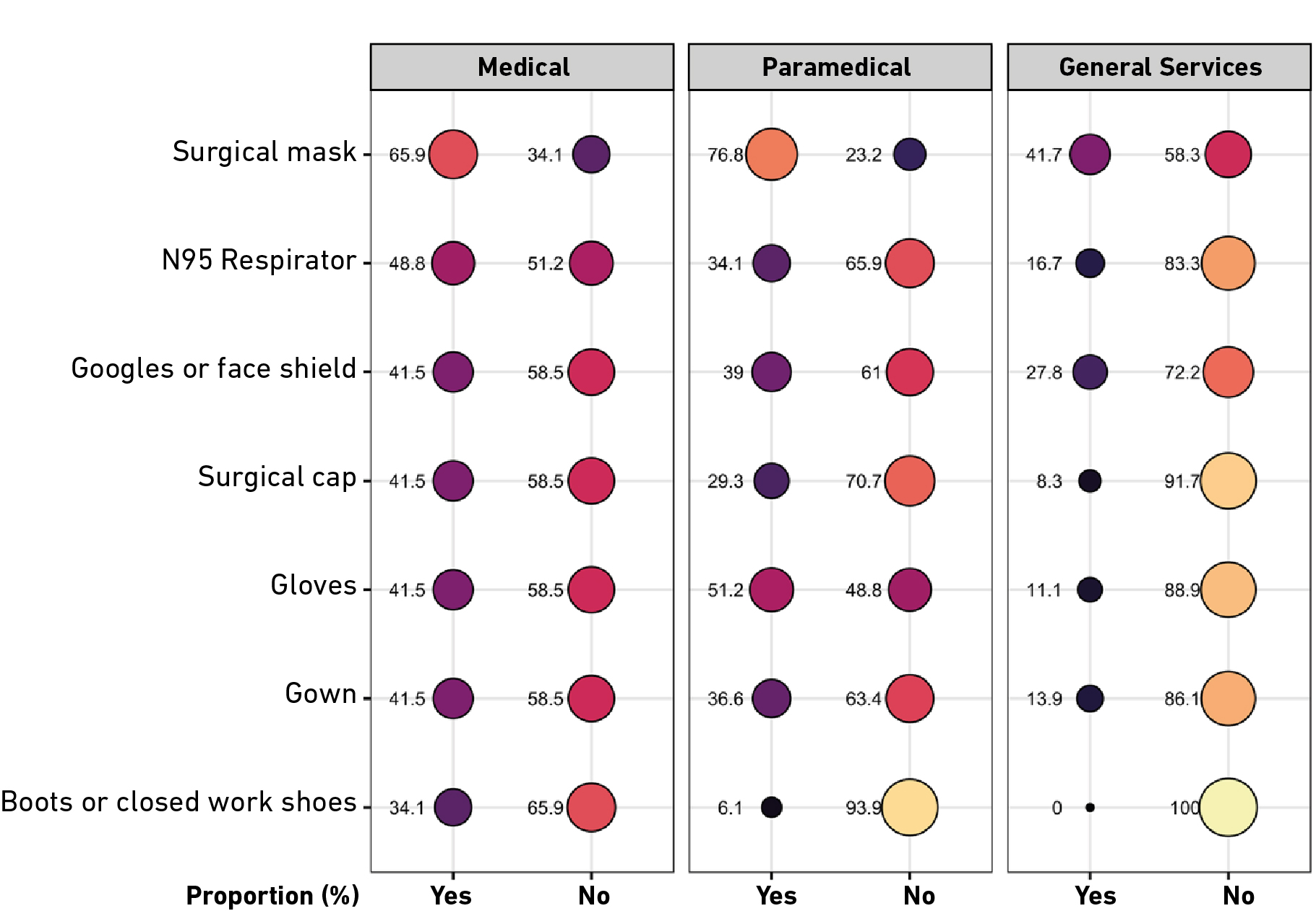
Results. The sample included females (57.2%) and paramedical staff (51.6%). The most commonly provided protective equipment was surgical masks. Healthcare workers showed an increased prevalence of obesity, hypertension, and diabetes. Statistically significant differences between the medical, paramedical, and general services departments regarding training and distribution of protective equipment (p<0.05) were identified. Low satisfaction concerning quality of working life and a low perception of safety with significant differences (p<0.05) were reported.
Conclusions. Further need for interventions and policies designed to prevent risks and improve health and well-being of healthcare workers in crisis situations is noted.
Keywords
Occupational health; healthcare workers; workplace safety; quality of work life; mental health; COVID-19.
Resumen
Introducción. La pandemia por COVID-19 creó un escenario de vulnerabilidad para los trabajadores de la salud, cuyas condiciones laborales y de salud se vieron afectadas por la alta demanda de atención a pacientes infectados con el virus SARS-CoV-2 en el entorno hospitalario, lo que alteró las condiciones de salud ocupacional en diversas áreas.
Objetivo. Analizar las condiciones de salud ocupacional en trabajadores de la salud de un hospital de segundo nivel durante el primer año de la pandemia por COVID-19.
Método. Estudio cuantitativo de alcance observacional y retrospectivo con una muestra de 159 trabajadores de la salud de una clínica hospital de segundo nivel. Se aplicó un instrumento de 103 ítems distribuidos en cinco secciones integradas por las variables sociodemográficas, laborales y de salud, así como también las relacionadas con la salud ocupacional. La metodología estadística consistió en análisis univariado para describir a la población de estudio, bivariado para la diferencia de proporciones y multivariado para la reducción de variables. El análisis y visualización de los datos se realizó en el software de programación estadística R Studio, versión 4.0.3.
Resultados. La muestra estuvo principalmente integrada por mujeres (57.2%) y personal de la rama paramédica (51.6%). El personal de salud mostró un aumento en la prevalencia de obesidad, hipertensión y diabetes. El equipo de protección que más se otorgó fue el cubrebocas quirúrgico. El personal de salud presentó estadísticamente significativas entre las ramas médica, paramédica y servicios generales en relación con la capacitación y distribución de los recursos de protección (p<0.05). Se presenta una baja satisfacción con la calidad de vida laboral y una baja percepción de seguridad con diferencias significativas (p<0.05).
Conclusiones. Se subrayan la necesidad de intervenciones y políticas destinadas a prevenir riesgos y mejorar la salud y el bienestar de los trabajadores de la salud en situaciones de crisis. Una alta prevalencia de obesidad, hipertensión arterial y diabetes.
Palabras clave
Salud ocupacional; trabajadores de la salud; seguridad en el trabajo; calidad de vida laboral; salud mental; COVID-19.
Introduction
In 2019, the COVID-19 pandemic originated in Wuhan, China, when deaths due to pneumonia of unknown etiology were reported. Subsequently, the coronavirus responsible for severe acute respiratory syndrome, named SARS-CoV-2, was identified [1]. The first case of COVID-19 in Mexico was detected in March 2020. Hence, the Mexican government implemented control phases to prevent the spread of this virus, including lockdowns on the public, private, and social sectors [2]. States were encouraged to define hospital reconversion plans to ensure timely health care for COVID-19 cases, considering health system activities as essential [3].
In this context, occupational accidents and work-related diseases have posed a concern for health systems, as they cause economic, social, and mental impacts and result in economic losses due to disabilities and/or loss of working life years. Occupational health, as defined by the World Health Organization (WHO), the promotion and maintenance of the highest degree of physical, mental and social well-being of workers in all occupations through the prevention of health deviations, risk control and the adaptation of work to people, and people to their jobs [4]. Moreover, health organizations must deal with psychosocial impacts, which directly exert influence on the quality of health care delivery [5]. The Job Demands-Resources Model states that maintaining a balance between the work environment and available resources is a determinant that affects occupational health. This model seeks to explain how multiple risks at work affect in terms of economic losses, mental health and even the quality of care provided to patients [6].
In Mexico, healthcare workers are in occupational settings with a high potential for exposure to COVID-19, classified as an occupational disease [7]. 283,122 cumulative COVID-19 cases were reported nationwide, with nursing staff accounting for 38.9%, physicians 25.3% and other health professionals 32%. Of the 4,517 confirmed deaths, 45% occurred among medical personnel, 19% among nursing staff, and 31% among other professionals [8].
Healthcare workers in close contact with infected patients were reported to experience symptoms of distress, depression, anxiety, and insomnia, attributable to the risk of contagion, feelings of vulnerability or loss of control, concerns about personal and family health, the spread of the virus, work changes, and isolation [9]. From a psychosocial perspective, the Demand-Control Model and the Effort-Reward Imbalance Model highlight that in work environments with high demands, limited control, or insufficient rewards, stress and anxiety levels tend to increase. This is particularly evident during crises such as the COVID-19 pandemic, where work overload and a shortage of personal protective equipment (PPE) exacerbated stress and anxiety [10,11]. In addition, we identified that the front-line nursing staff experienced the highest levels of anxiety, stress, and depression, which were mainly related to the shortage of PPE, followed by a lack of technological equipment and human resources [12].
Additionally, ergonomic occupational risks were identified, with more than 70% of workers experiencing muscle pain or sprains and 56% reporting posture problems. Among physical hazards, the most common were slips and falls, forced postures, and repetitive activities [13-15].
The interaction between workers and their activities during contingency affected their performance and quality of working life. Several studies have shown that the lack of PPE during the COVID-19 pandemic resulted in increased fear [12,16]. On the other hand, Wauters et al. reported that institutional support, proper implementation of safety protocols, work organization, and training are protective factors that contribute to maintaining a favorable work environment and satisfactory quality of life [16].
However, it has been observed that healthcare workers in healthy work environments show high levels of work engagement, strive for excellent patient care and improve care quality techniques, even in difficult situations [17,18]. This study focused on the secondary level of care, as it experienced a higher demand for medical services. Patients with complications from the disease required hospitalization and specialized management, which extended their hospital stays and increased the workload and altered occupational health. Therefore, the objective of this research was to analyze the occupational health conditions of healthcare workers in a secondary care hospital during the first year of the COVID-19 pandemic to explore their working conditions to improve and promote safe and healthy work environments. The hypothesis that guided the research is that during the first year of the COVID-19 pandemic, healthcare workers in a secondary care hospital experienced poor occupational health conditions, including physical and mental health problems, high musculoskeletal risks, low quality of work life, and unsatisfactory perceptions of workplace safety.
Method
Design and Context
We conducted a quantitative, observational, and retrospective study. The target population included healthcare personnel from medical, paramedical, and general services departments who worked during the first year of the COVID-19 pandemic (2020) at a secondary care hospital clinic that delivers health services to government workers and is located in the state of Veracruz, Mexico.
Participants
The population size consisted of 673 workers; the sample was determined using the formula for finite populations with a 95% confidence interval and a 7% margin of error. This margin was chosen due to continuing restrictions, as the hospital had been converted to care for COVID-19 patients and the data collection period was limited. A total of 159 workers were included in the sample, selected through random sampling. Inclusion criteria required participants to have worked during the first year of the COVID-19 pandemic for more than six months.
Tools and Variables
Healthcare workers participated in a survey for data collection using a 103-item questionnaire, which included an informed consent section and five domains:
1) Sociodemographic characteristics: Health (diseases or risk conditions, occupational accidents, and work-related diseases) and work (job role, type of personnel, employment history, etc.). 2) Job satisfaction and quality of working life: A 31-item questionnaire with seven domains assessed satisfaction levels as low (≤ 40th percentile) or high (≥ 60th percentile) for variable analysis. Validation was conducted through expert consultation and Exploratory Factor Analysis (EFA), complemented by relevant validity using the average square root of communality (0.68). Reliability was measured with Cronbach’s Alpha (α = 0.95) [19]. 3) Occupational safety climate: A 29-item Nordic Occupational Safety Climate Questionnaire assessing safety perception on a low-to-high scale. Validation through EFA explained 84.6% of total variance, with reliability measured as α = 0.88 [20]. 4) Mental health: The Depression, Anxiety, and Stress Scale (DASS), including seven items per subscale, was quantitatively assessed by average scores for each domain. EFA with varimax rotation explained 46.6% of total variance, and reliability was α = 0.86 [21]. 5) Musculoskeletal symptoms: The Standardized Nordic Questionnaire explored pain in 11 body areas using "yes" or "no" responses. EFA explained 72.5% of total variance, and reliability was α = 0.86 [22]. All questionnaires were standardized and validated for the Mexican population.
Data Processing and Analysis
Microsoft Excel for Mac (version 16.69.1) was used for data cleaning and coding. The normality assumption was tested using the Kolmogorov-Smirnov test, as the sample size exceeded 30 participants. Since the continuous variables did not meet the normality assumptions, nonparametric tests were used to compare the continuous occupational health variable. Univariate analyses were conducted for descriptive statistics (frequencies and proportions) and measures of central tendency. Bivariate analyses were conducted for group comparisons, using the chi-square test for categorical variables. For comparisons of the continuous variable across more than two independent groups, the nonparametric Kruskal-Wallis test was applied. Finally, a multivariate analysis was conducted to reduce the dimensions of analysis and generate the new occupational health variable. The categorical principal components technique was employed, as it was suitable for the nominal and ordinal measurement scales of the instruments. The instruments mentioned above were selected based on a literature review, and the decision to include them in this study was based on a review by expert researchers in occupational health. No adjustments were made for complementary variables during the creation of the new variable. This new variable was elaborated considering tools 2 to 5 and measured from 1 to 100, with the higher score, the better occupational health. The open-source R Studio software (version 4.0.3) was used for analysis and graphical representation. No missing values were identified in the statistical analyses.
Ethical Considerations
This research was approved by the Health Sciences Research Board, with reference number M182/2023, and the Ethics Board of Instituto de Salud Pública, attached to Universidad Veracruzana, with reference number CEI-ISP-UV-R08/2023. Additionally, a "No Coercion" form and approval from the Teaching and Research Coordination of the Hospital Clinic were obtained with reference number 002/038/466.
Results
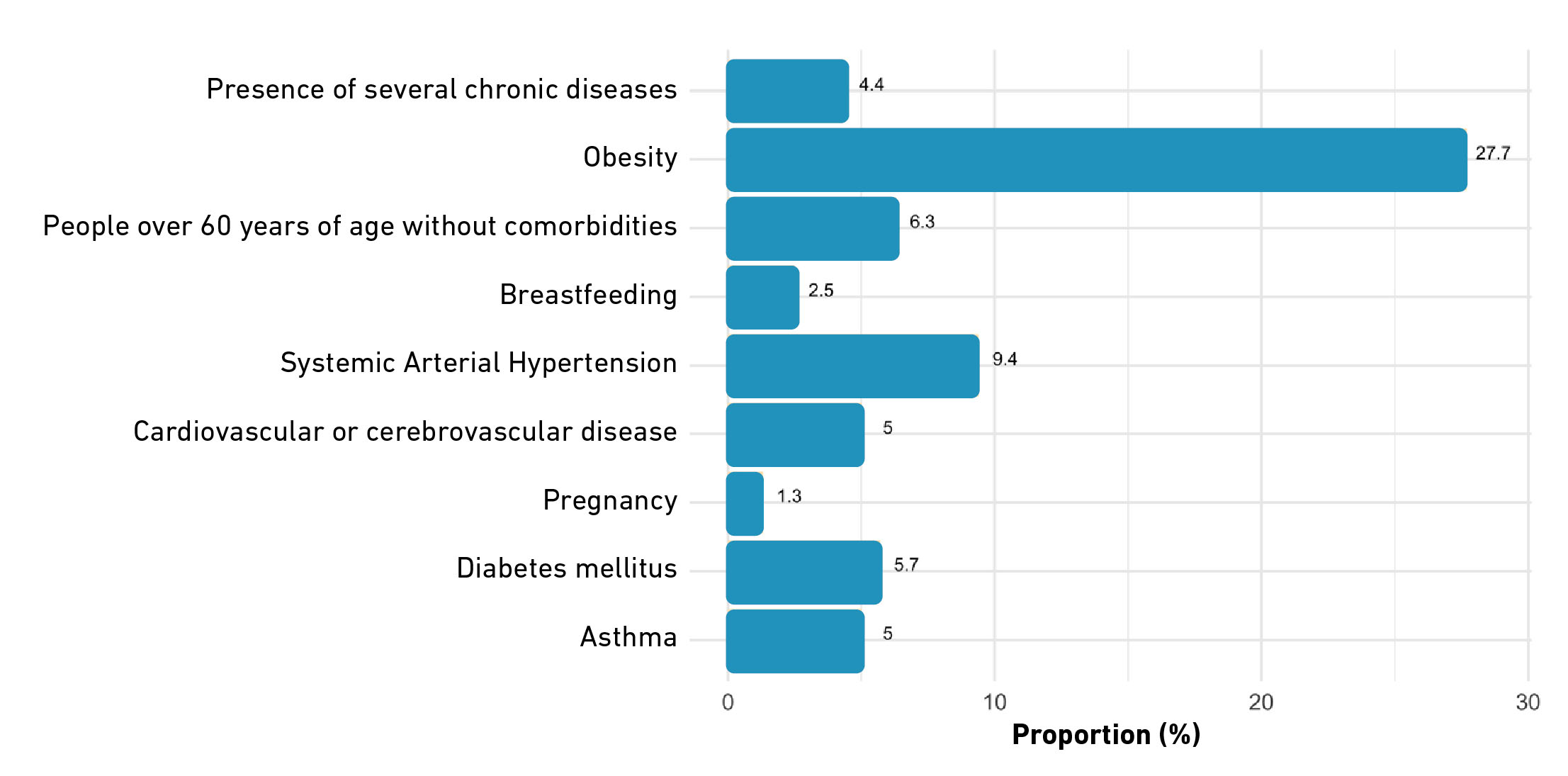
The final sample included 159 workers, predominantly females (57.2%) with an average age of 45 ± 12 years. Most of them were career civil service personnel (Table 1). A total of 42.8% self-reported having a condition or disease that may result in COVID-19 (Figure 1).
Table 1. Sociodemographic and occupational characteristics for health workers.
| Variable | Frequency | % |
|---|---|---|
| Sex | ||
| Female | 91 | 57.2 |
| Male | 68 | 42.8 |
| Schooling | ||
| Basic | 3 | 1.9 |
| Secondary | 41 | 25.8 |
| Higher | 115 | 72.3 |
| Marital status | ||
| Single | 101 | 63.5 |
| Married | 58 | 36.5 |
| Jobs | ||
| Health administration | 60 | 37.7 |
| Physician | 35 | 22 |
| General Nurse/Specialist | 20 | 12.6 |
| Nursing Assistant | 16 | 10.1 |
| Laboratory Technician | 4 | 2.5 |
| Dietician | 4 | 2.5 |
| Stretcher-bearer | 3 | 1.9 |
| Othera | 17 | 10.7 |
| Type of staff | ||
| Career civil servants | 85 | 53.5 |
| Trust officers | 30 | 18.9 |
| Interim / interim officers | 44 | 27.7 |
| Employment history | ||
| < 15 years old | 104 | 65.4 |
| 15 to 30 years old | 29 | 18.2 |
| > 30 years | 26 | 16.4 |
| Work shift | ||
| Morning | 73 | 45.9 |
| Evening | 18 | 11.3 |
| Diurnal | 13 | 8.2 |
| Nocturnal | 23 | 14.5 |
| Discontinuous | 32 | 20.1 |
| Departments | ||
| Medical | 41 | 25.8 |
| Paramedical | 82 | 51.6 |
| General Services | 36 | 22.6 |
| Multiple jobholding | ||
| Yes | 22 | 13.8 |
| No | 137 | 86.2 |
| Received PPE | ||
| Yes | 118 | 74.2 |
| No | 41 | 25.8 |
| Received COVID-19 training | ||
| Yes | 74 | 46.5 |
| No | 85 | 53.5 |
| Risk condition or disease | ||
| Yes | 68 | 42.8 |
| No | 91 | 57.2 |
| Workplace Accident | ||
| Yes | 7 | 4.4 |
| No | 152 | 95.6 |
| Occupational disease | ||
| Yes | 16 | 10.1 |
| No | 143 | 89.9 |
Note. a Regarding jobs, "Other" refers to Pharmacy Officer and/or Dispatcher, Chemist, Social Worker, Cook, Psychologist, Medical Supervisor, Respiratory therapist, Medical Diagnostic Assistant, Head of Statistics and Outpatient Consultation and Nursing Education Coordinator.
Figure 1. Proportion of workers with a condition or disease at risk for COVID-19.
Table 2 contains a comparison between the different departments showing that during the first year of the pandemic the medical department was mostly males (56.1%). In contrast, women predominated in the paramedical department (67.1%), while the general services department showed equal proportions for males and females. A statistically significant difference was identified between sex groups and departments (p<0.05).
Table 2. Comparison of sociodemographic and labor characteristics by departments.
| Variable | Medical | Paramedical | Services General | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Sex | |||||||
| Female | 18 | 43.9 | 55 | 67.1 | 18 | 50 | 0.030 |
| Male | 23 | 56.1 | 27 | 32.9 | 18 | 50 | |
| Schooling | |||||||
| Basic | 0 | 0 | 0 | 0 | 3 | 8.3 | p<0.001 |
| Secondary | 0 | 0 | 31 | 37.8 | 10 | 27.8 | |
| Higher | 41 | 100 | 51 | 62.8 | 23 | 63.9 | |
| Marital status | |||||||
| Single | 37 | 90.2 | 46 | 56.1 | 18 | 50 | p<0.001 |
| Married | 4 | 9.8 | 36 | 43.9 | 18 | 50 | |
| Children | |||||||
| No children | 38 | 92.7 | 26 | 31.7 | 6 | 16.7 | p<0.001 |
| With children | 7 | 7.3 | 56 | 68.3 | 30 | 83.3 | |
| COVID Training | |||||||
| Yes | 11 | 26.8 | 54 | 65.9 | 9 | 25 | p<0.001 |
| No | 30 | 73.2 | 28 | 34.1 | 27 | 75 | |
| Received PPE | |||||||
| Yes | 33 | 80.5 | 66 | 80.5 | 19 | 52.8 | 0.004 |
| No | 8 | 19.5 | 16 | 19.5 | 17 | 47.2 | |
| Risk condition or disease | |||||||
| Yes | 26 | 63.4 | 34 | 41.5 | 8 | 22.2 | 0.001 |
| No | 15 | 36.6 | 48 | 58.5 | 28 | 77.8 | |
| Workplace Accident | |||||||
| Yes | 3 | 7.3 | 4 | 4.9 | 0 | 0 | 0.282 |
| No | 38 | 92.7 | 78 | 95.1 | 36 | 100 | |
| Occupational disease | |||||||
| Yes | 10 | 24.4 | 3 | 3.7 | 3 | 8.3 | 0.001 |
| No | 31 | 75.6 | 79 | 96.3 | 33 | 91.7 | |
Note. b Comparison of proportions using the Chi-square test with a significance level of p<0.05.
The general services department showed a lower proportion of personnel who received PPE (52.8%) compared to the medical and paramedical departments (Figure 2). Regarding self-reported occupational diseases, the medical department showed a higher proportion (24.4%). Statistically significant differences in proportions were identified between the mentioned variables and the different departments (p<0.05) (Table 2).
Figure 2. Proportion of PPE provided by departments.
Regarding COVID-19 training, the paramedical department reported the highest proportion of trained personnel (65.9%), while more than 70% of the medical and general services departments reported not being trained, resulting in a statistically significant difference (p<0.001) (Table 2).
Concerning the variables considered to explore occupational health, Table 3 shows a comparison between the different departments. Low satisfaction with quality of work life predominated among medical and general services departments. However, the medical department showed the highest proportion (63.4%), while more than 40% of paramedical department experienced high satisfaction (43.9%). These findings revealed a significant difference between satisfaction with quality of work life and the departments (p<0.001).
Table 3. Comparison of variables to explore occupational health by departments.
| Variable | Medical | Paramedical | General Services | ||||
|---|---|---|---|---|---|---|---|
| No or Mc | % or Q1-Q3c | No M | % or Q1-Q3 | No M | % or Q1-Q3 | ||
| Satisfaction with quality of working life | |||||||
| Low | 26 | 63.4 | 22 | 26.8 | 13 | 36.1 | p<0.001 |
| Medium | 0 | 0 | 24 | 29.3 | 13 | 36.1 | |
| High | 15 | 36.6 | 36 | 43.9 | 10 | 27.8 | |
| Perception of safety environment | |||||||
| Low | 17 | 41.5 | 48 | 58.5 | 17 | 47.2 | 0.015 |
| Quite low | 10 | 24.4 | 9 | 11 | 12 | 33.3 | |
| Very high | 7 | 17.1 | 6 | 7.3 | 5 | 13.9 | |
| High | 7 | 17.1 | 19 | 23.2 | 2 | 5.6 | |
| Physical discomfort | |||||||
| Yes | 24 | 58.5 | 38 | 46.3 | 18 | 50 | 0.443 |
| No | 17 | 41.5 | 44 | 53.7 | 18 | 50 | |
| Mental health | |||||||
| Stress | 4 | 3.6-7.9 | 2 | 2.8-4.9 | 2.5 | 3.3-6.6 | 0.169 |
| Anxiety | 5 | 3.9-8.0 | 1 | 2.6-4.6 | 3 | 2.6-5.6 | 0.041 |
| Depression | 2 | 3.0-7.2 | 1 | 2.2-4.0 | 4 | 3.4-6.5 | 0.078 |
Note 1. c For the categorical variables of satisfaction with the quality of working life, perception of a safe environment and physical discomfort, absolute frequencies (n) and percentage of the proportion (%) were used. While for the continuous variable of mental health, the median (M) and the Interquartile Pathway (Q1-Q3) were used.
Note 2. d Comparison of proportions using the Chi-square test for categorical variables and mean difference using the Kruskal-Wallis test with a significance level of p<0.05 for both cases.
Additionally, the difference in proportions between safety perception and departments was statistically significant (p<0.05). However, all three groups had a low perception of safety, with 80.5% of general services department perceiving a low or very low safety environment. It is noted that a considerable proportion of the paramedical department reported perceiving a high safety environment (23.2%).
Regarding physical discomfort, the paramedical department showed a higher proportion with no discomfort in any body area (53.7%), while the medical department was the most affected (58.5%), with the same proportion found in the general services department. No statistically significant difference was identified (p>0.05) (Table 3).
In the same way, no difference was identified between medians for stress and depression scores (p>0.05). However, the medical department showed higher scores for the stress variable, while the general services department showed the highest median for the depression variable. Nonetheless, the medical department showed the highest score for the anxiety variable, while the paramedical department showed the lowest score. Thus, a statistically significant difference was found between anxiety medians and departments (p<0.05).
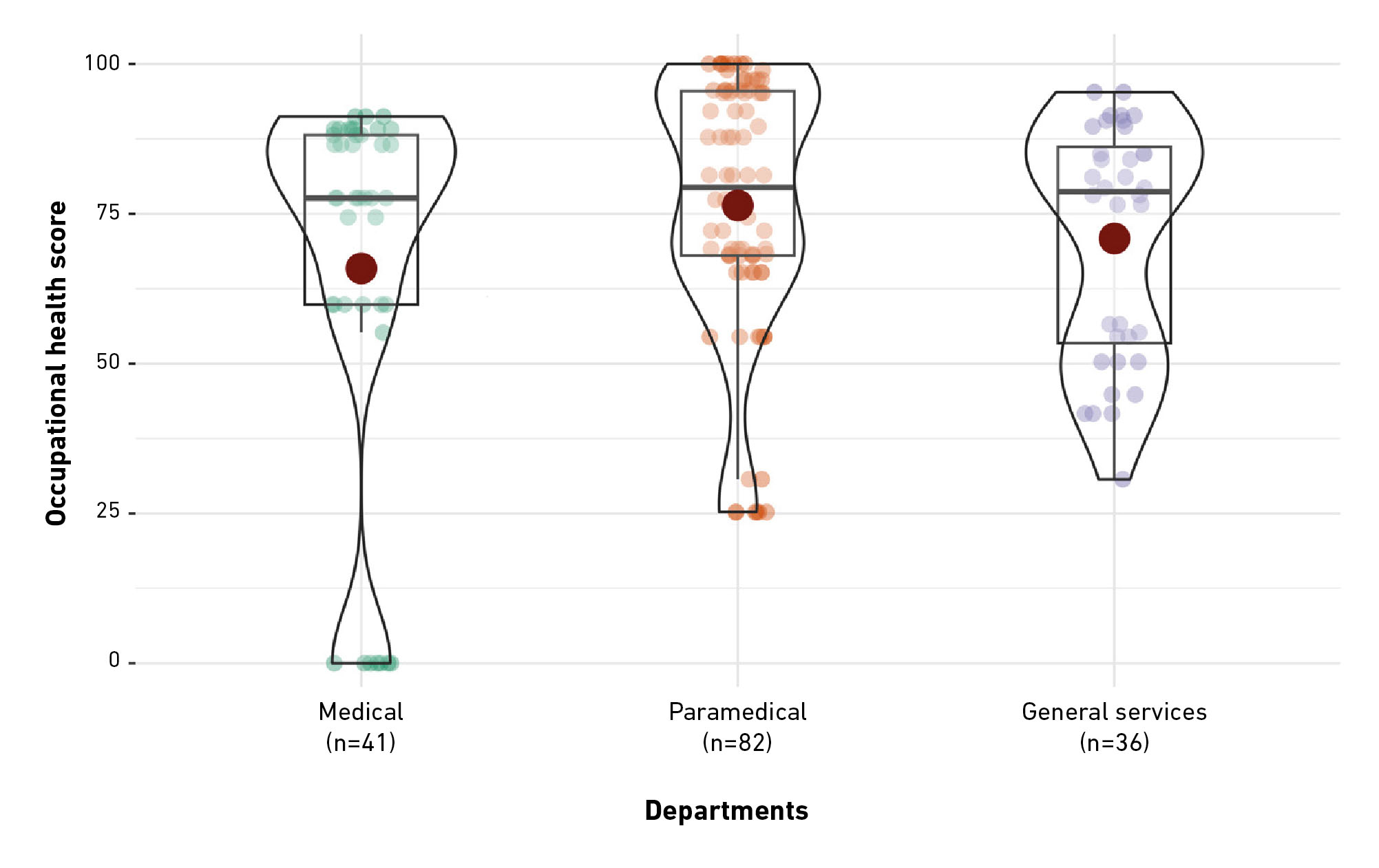
Figure 3 shows the transformed occupational health variable, with violin plots wider at the top due to the density of observations, which exceed 80 points for all three departments. The highest median for occupational health was achieved by the paramedical department with 79.4 (IQR: 71.6 - 81.1), followed by general services department with 78.7 (IQR: 64.3 - 79.4). In contrast, the medical department had a lower median with 77.6 (IQR: 55.8 - 76.0), along with greater data dispersion.
Figure 3. Comparison of occupational health scores by departments.
Despite the differences in medians and dispersion, the Kruskal-Wallis test revealed no significant differences between groups (H (3) = 0.092, p > 0.05). Therefore, occupational health scores showed no significant variations for departments.
Discussion
This study analyzed the occupational health conditions among healthcare personnel during the first year of the pandemic. We found low satisfaction with the quality of work life among the medical and general services departments, as well as low and very low levels of safety perception in the work environment. Moreover, an unequal distribution of PPE and COVID-19 training was identified, resulting in statistically significant differences between the departments.
Regarding professional development inside of the institution, a considerable proportion of medical and general services workers did not receive COVID-19 training, as reported by Mera-Mamián et al. [23], where more than 50% of the personnel stated that training was limited or absent.
On the other hand, the literature has reported that PPE is one of the scarce resources. However, this study found that the most disadvantaged department was that of the general services compared to the medical and paramedical departments, which exceeded 80% of their staff receiving PPE [12]. The surgical mask, with more than 60%, was the most commonly used PPE across all staff, consistent with other studies where the proportion was similar [23-24].
Regarding the availability of PPE, unequal distribution was reported in Peru, the healthcare workers without contracts received less PPE compared to those with permanent contracts. Additionally, younger workers were found to receive incomplete PPE compared to those over 55 years of age [24]. The authors suggested that full PPE was prioritized for older adults due to their higher vulnerability to COVID-19. This corresponds to the measures taken by Mexico, where individuals aged 60 and above were considered at higher risk for complications from COVID-19 [7]. Shortages of PPE were associated with a decline in mental health and emotional exhaustion, particularly among frontline healthcare workers.
Concerning health characteristics, approximately 43% of healthcare personnel reported having a condition or disease that posed a risk for them. This proportion was similar to what was reported by Delgado-Valencia et al. [25], in 2020, where 45.5% of workers indicated having a chronic disease. The most prevalent conditions were obesity, hypertension, and diabetes mellitus.
Regarding hypertension, other studies on the Mexican population have found a higher prevalence up to 13%. For obesity, the sample analyzed in this study had a higher prevalence of 12%, while for diabetes mellitus the prevalence observed was similar to what has been reported in other studies among physicians and nursing personnel [25-27].
According to the analyzed variables regarding occupational health, low satisfaction with the quality of work life prevailed among the medical and general services departments. These results differ from those found by other authors in Latin America, since they have reported that more than 65% of healthcare personnel were moderately satisfied with their quality of working life [28,29]. Moreover, other studies have highlighted that training and institutional support are factors that contribute to satisfaction with quality of working life and creating a beneficial environment for professional development [16].
This could be attributed to the level of institutional support received, as these two types of personnel showed similar outcomes for training and PPE provision. Moreover, training was identified as an essential resource requiring reinforcement, as access to specific knowledge enhances the response to health emergencies. Conversely, inadequate training undermines healthcare workers' confidence in their ability to provision quality care [30,31]. Likewise, a study in the United Kingdom found that healthcare workers redeployed during staff shortages and lacking adequate, or any training were significantly more probable to experience symptoms of post-traumatic stress disorder [32].
Additionally, more than 40% of healthcare personnel perceived a low safety environment within the hospital. It is noteworthy that this situation predominantly affected the paramedical and general services departments. Interestingly, these departments had a higher proportion of personnel with children, which could imply greater sensitivity toward safety issues. The literature indicates that the fear of infecting a family member was a relevant factor contributing to the experience of fear and anxiety when working with infected patients [9,12].
A systematic review found that low-resource countries, healthcare workers experienced low satisfaction with the infrastructure and poorly ventilated rooms, as well as the poor conditions of isolation rooms for infected patients and the lack of institutional support to provide the correct PPE which put his physical and mental health at risk [33]. These results are in line with what is found in the literature, where low and very low safety levels are most common among healthcare personnel who worked during the COVID-19 pandemic [34,35].
Regarding physical discomfort, it has been reported that medical department show a higher prevalence of physical discomfort (pain), ranging from 60% to 80%, while the paramedical personnel show a lower prevalence [36]. The findings of this study are consistent with this, as the medical department was the most affected (58.5%). Additionally, this group also had a higher proportion of individuals with some condition or disease, as well as with occupational accidents and work-related diseases. It is important to highlight that musculoskeletal disorders (MSDs) are among the leading causes of disability worldwide [37]. Besides, a statistically significant association has been identified between MSDs and lack of physical activity (p = 0.024) [38]. In the same way, a high Muscle Mass Index has been associated with increased odds of developing low back pain, which is particularly relevant given that 27.7% of the healthcare workers in this study reported obesity [39].
Concerning mental health, the medical department showed the highest medians on the stress and anxiety subscales, while the general services department showed the highest scores on the depression subscale. However, it is important to note that these scores were below those reported by other studies [40]. It is noted that departments had the highest proportion of personnel who received no training, which could have negatively influenced and increased the scores in the mental health domain. This is relevant given that at the beginning of the pandemic, healthcare workers were concerned about infection prevention and control guidelines, as well as the uncertainty in treating COVID-19 patients [12,41]. A systematic review highlighted that workplace well-being interventions, significantly improved work engagement and quality of life while reducing emotional exhaustion and symptoms of stress, anxiety and depression. Relaxation techniques were identified as the most used strategies due to their facility of implementation [42]. Resilience-building strategies in health organizations during crises include staff training and promote collaboration with senior staff. These practices could strengthen well-being, which should be integrated into health workforce training programs [43].
Conclusions
The result of this study highlights significant disparities in occupational health conditions among health care departments, particularly affecting medical and general service personnel. Low levels of quality of life and perception of safety were observed in these groups, with general service personnel receiving a lower proportion of PPE compared to other departments, which shows inequalities in the allocation of resources. Just like, the unequal distribution of training and resources indicate the vulnerability of a significant part of the labor force.
Mental health impacts were most pronounced among medical and general services department, emphasizing that need for objective interventions. In addition, medical department reported the lowest scores in occupational health, reflecting their greater vulnerability during crisis situations. These findings emphasize the importance of implementing targeted programs focused on training, mindfulness, the promotion of healthy habits, and physical activity to improve the well-being and resilience of healthcare workers. In addition, continuing monitoring and support are essential to address inequality and improving occupational health.
This study is noted for analyzing several occupational health variables, as statistical analyses were done for type of personnel and used a robust multivariate analysis. These strengths help identify inequalities and propose an innovative perspective for further research. However, possible limitations include memory bias typical in its retrospective approach and the lack of stratification in the sampling by personnel and gender, which prevented us from obtaining a fully representative sample.
References
1. Lu H, Stratton CW, Tang Y. Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J Med Virol [Internet]. 2020;92(2):401-2. doi: https://doi.org/10.1002/jmv.25678
2. Suárez V, Suarez Quezada M, Oros Ruiz S, Ronquillo De Jesús E. Epidemiología de COVID-19 en México: del 27 de febrero al 30 de abril de 2020. Revista Clínica Española [Internet]. 2020(8);220:463-71. doi: https://doi.org/10.1016/j.rce.2020.05.007
3. Acuerdo por el que se establecen acciones extraordinarias para atender la emergencia sanitaria generada por el virus SARS-CoV2. Diario Oficial de la Federación No. 36 (Mar 31, 2020). Available from: https://www.dof.gob.mx/nota_detalle.php?codigo=5590914&fecha=31/03/2020
4. Panamerican Health Organization (PAHO) [Internet]. Washington: PAHO/WHO; c2022. Salud de los Trabajadores: Recursos - Preguntas Frecuentes; [retrieved 2022 Jan 1; cited 2022 Jan 1]; [about 6 screens]. Available from: https://web.archive.org/web/20220301230114/https://www3.paho.org/hq/index.php?option=com_content&view=article&id=1527:workers-health-resources&Itemid=1349&limitstart=2&lang=es
5. Cruz-Ausejo L, Vera-Ponce VJ, Torres-Malca JR, Roque-Quesada JC. Occupational accidents in healthcare workers: a bibliometric analysis in Scopus database 2010-2019. Rev Bras Med Trab [Internet]. 2023;20(4):642-9. doi: https://doi.org/10.47626/1679-4435-2022-724
6. Bakker AB, Demerouti E. The Job Demands‐Resources model: state of the art. Journal of Managerial Psychology [Internet]. 2007;22(3):309-28. doi: https://doi.org/10.1108/02683940710733115
7. Instituto Mexicano del Seguro Social. Circular No. 09 90 01 300000. Criterios de calificación para casos con coronavirus (COVID-19) como Enfermedad de Trabajo (Apr 6, 2020). Available from: https://www.imss.gob.mx/sites/all/statics/COVID-19/documentos/2021-01-Ofc_068_ ET.pdf
8. Secretaría de Salud [Internet]. Ciudad de México: Gobierno de México; c2024. Informes sobre el personal de Salud COVID19 en México 2021; [updated 2021 Oct 28; cited 2022 Dec 11]; [about 5 screens]. Available from: https://www.gob.mx/salud/documentos/informes-sobre-el-personal-de-salud-covid19-en-mexico-2021
9. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw Open [Internet]. 2020;3(3):e203976. doi: https://doi.org/10.1001/jamanetworkopen.2020.3976
10. Kain J, Jex S. Karasek’s (1979) job demands-control model: A summary of current issues and recommendations for future research. In Perrewé PL, Ganster DC, editors. New Developments in Theoretical and Conceptual Approaches to Job Stress (Research in Occupational Stress and Well Being, Vol. 8) [Internet]. Bingley: Emerald Group Publishing Limited; 2010. p. 237-68. doi: https://doi.org/10.1108/S1479-3555(2010)0000008009
11. Siegrist J. Chapter 9 - Effort-Reward Imbalance Model. In Fink G, editor. Stress: Concepts, Cognition, Emotion, and Behavior. Handbook of Stress Series Volume 1 [Internet]. London: Academic Press; 2016. p. 81-6. doi: https://doi.org/10.1016/B978-0-12-800951-2.00009-1
12. Sánchez Díaz JS, Peniche Moguel KG, Rivera Solís G, González Escudero EA, Martínez Rodríguez EA, Monares Zepeda E, et al. Psicosis del personal de salud en tiempos de COVID-19. Med Crit [Internet]. 2020;34(3):200-3. doi: https://doi.org/10.35366/94900
13. Moitra M, Rahman M, Collins PY, Gohar F, Weaver M, Kinuthia J, et al. Mental Health Consequences for Healthcare Workers During the COVID-19 Pandemic: A Scoping Review to Draw Lessons for LMICs. Front Psychiatry [Internet]. 2021;12:1-10. doi: https://doi.org/10.3389/fpsyt.2021.602614
14. Hamid A, Salaam Ahmad A, Dar S, Sohail S, Akram F, Irfan Qureshi M. Ergonomics Hazards and Musculoskeletal Disorders Among Workers of Health Care Facilities. Curr World Environ [Internet]. 2018;13(2):251-8. doi: https://doi.org/10.12944/CWE.13.2.10
15. Luengo Martínez C, Ortiz Pino I, Loyola Salas C. Accidentes Laborales no cortopunzantes Notificados en Trabajadores de un Hospital de la Red de Salud Pública, Chile 2014-2016. Archivos de Medicina [Internet]. 2019;19(2):313-19. doi: https://doi.org/10.30554/archmed.19.2.3297.2019
16. Wauters M, Zamboni Berra T, de Almeida Crispim J, Arcêncio RA, Cartagena-Ramos D. Calidad de vida del personal de salud durante la pandemia de COVID-19: revisión exploratoria. Rev Panam Salud Pública [Internet]. 2022;46:1-9. doi: https://doi.org/10.26633/RPSP.2022.30
17. Fernández Merino C, Yáñez Gallardo R. Describiendo el engagement en profesionales de enfermería de atención primaria de salud. Cienc enferm [Internet]. 2014;20(3):131-40. doi: https://doi.org/10.4067/S0717-95532014000300012
18. Bakker AB, Demerouti E, Sanz-Vergel AI. Burnout and Work Engagement: The JD-R Approach. Annual Reviews [Internet]. 2014;1:389-411. doi: https://doi.org/10.1146/annurev-orgpsych-031413-091235
19. González-Baltazar R, Hidalgo-Santacruz G, Salazar-Estrada JG, Preciado-Serrano M del L. Elaboración y Validación del Instrumento para Medir Calidad de Vida en el Trabajo “CVT-GOHISALO.” Cienc Trab. 2010;12(36):332-40.
20. Jaimes-Hernández DA, Vargas-Hernández MA. Validación del cuestionario nórdico de clima de seguridad NOSACQ 50, en empresas de diversos sectores [master’s tesis]. [Bogotá]: Pontificia Universidad Javeriana. 2019; 187 p. doi: https://doi.org/10.11144/Javeriana.10554.46261
21. Gurrola-Peña GM, Balcázar-Nava P, Bonilla-Muños MP, Virseda-Heras JA. Estructura factorial y consistencia interna de la escala de Depresión, Ansiedad y Estrés (DASS-21) en una muestra no clínica. Psicología y Ciencia Social. 2006;8(2):3-7.
22. González Muñoz EL. Estudio de validez y confiabilidad del cuestionario nórdico estandarizado, para detección de síntomas musculoesqueléticos en población mexicana. EID [Internet]. 2021;3(1):8-17. doi: https://doi.org/10.29393/EID3-1EVEG10001
23. Mera-Mamián A, Delgado-Noguera M, Merchán-Galvis Á, Cabra G, Calvache JA. Conocimientos y necesidades del personal de salud sobre elementos de protección personal durante la pandemia por COVID-19 en el Cauca. Rev Fac Cienc Salud Univ Cauca [Internet]. 2020;22(1):16-23. doi: https://doi.org/10.47373/rfcs.2020.v22.1581
24. Raraz Vidal JG, Allpas Gomez HL, Torres Salome FK, Cabrera Patiño WM, Ramos Gómez RP, Alcántara Leyva LM, et al. Work conditions and personal protective equipment against COVID-19 in health personnel, Lima-Peru. Rev Fac Med Hum [Internet]. 2021;21(2):335-45. doi: https://doi.org/10.25176/RFMH.v21i2.3608
25. Delgado-Valencia CA, Bárcenas-Hernández B, Narváez-Velázquez B, Salas-Martínez MC, Hernández-López CI, Pérez-Gómez J, et al. Vacunación contra coronavirus 2019 y estrés laboral en el personal de enfermería. Rev CONAMED [Internet]. 2022;27(4):159-66. doi: https://doi.org/10.35366/108481
26. Villarreal-Barrios ZM, León-Garnica G, Mercado-Uribe MC, García-Benavides L, Yanowsky-Reyes G, Flores-Tinajero MA, et al. Diagnóstico situacional por COVID-19 e impacto en la salud de los médicos del Antiguo Hospital Civil de Guadalajara (AHCGFAA). Sal Jal [Internet]. 2023;10(1):15-21. doi: https://doi.org/10.35366/111180
27. Perez-Izquierdo LE, Rivera-García R, Villarreal-Ríos E, Ávalos-Córdova P, Galicia-Rodríguez L, Barragán-Montes E, et al. Incidencia de COVID-19 en trabajadores de salud. Actividad laboral y resguardo domiciliario. Rev Med Inst Mex Seguro Soc [Internet]. 2022;60(4):453-9. Available from: http://revistamedica.imss.gob.mx/editorial/index.php/revista_medica/article/view/4575
28. Meza Espinoza EM, Fretel Quiroz NM, Lema Rivera FF, Castro Galarza CR, Canchari Fierro YE, Velasquez Bernal LR. Calidad de vida laboral y desempeño del personal en un Hospital Materno Infantil del Perú. Vive [Internet]. 2023;6(16):129-41. doi: https://doi.org/10.33996/revistavive.v6i16.212
29. Adanaqué Castillo J, Reynoso Valdez A, Contreras Castro FL. Factores sociolaborales asociados a la calidad de vida en el trabajo del profesional de enfermería que labora en una clínica privada, Lima, 2020. RCCS [Internet]. 2020;13(1):59-66. doi: https://doi.org/10.17162/rccs.v13i1.1347
30. Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID-19 patients. Am J Infect Control [Internet]. 2020;48(6):592-8. doi: https://doi.org/10.1016/j.ajic.2020.03.018
31. Travers JL, Schroeder K, Norful AA, Aliyu S. The influence of empowered work environments on the psychological experiences of nursing assistants during COVID-19: a qualitative study. BMC Nurs [Internet]. 2020;19:98. doi: https://doi.org/10.1186/s12912-020-00489-9
32. Couper K, Murrells T, Sanders J, Anderson JE, Blake H, Kelly D, et al. The impact of COVID-19 on the wellbeing of the UK nursing and midwifery workforce during the first pandemic wave: A longitudinal survey study. Int J Nurs Stud [Internet]. 2022;127:104155. doi: https://doi.org/10.1016/j.ijnurstu.2021.104155
33. Chemali S, Mari-Sáez A, El Bcheraoui C, Weishaar H. Health care workers’ experiences during the COVID-19 pandemic: a scoping review. Hum Resour Health [Internet]. 2022;20(1):27. doi: https://doi.org/10.1186/s12960-022-00724-1
34. Moda HM, Dama FM, Nwadike C, Alatni BS, Adewoye SO, Sawyerr H, et al. Assessment of Workplace Safety Climate among Healthcare Workers during the COVID-19 Pandemic in Low and Middle Income Countries: A Case Study of Nigeria. Healthcare [Internet]. 2021;9(6):1-11. doi: https://doi.org/10.3390/healthcare9060661
35. AlMousa N, Althabet N, AlSultan S, Albagmi F, AlNujaidi H, Salama KF. Occupational Safety Climate and Hazards in the Industrial Sector: Gender Differences Perspective, Saudi Arabia. Front Public Heal [Internet]. 2022;10. doi: https://doi.org/10.3389/fpubh.2022.873498
36. Jacquier-Bret J, Gorce P. Prevalence of Body Area Work-Related Musculoskeletal Disorders among Healthcare Professionals: A Systematic Review. Int J Environ Res Public Health [Internet]. 2023;20(1):1-26. doi: https://doi.org/10.3390/ijerph20010841
37. James SL, Abate D, Abate KH, Abay SM, Abbafati C, Abbasi N, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet [Internet]. 2018;392(10159):1789-858. doi: https://doi.org/10.1016/S0140-6736(18)32279-7
38. Alruwaili SH, Thirunavukkarasu A, Alanazi RM, Alsharari AY, Alruwaili DK, Alenzi HA, et al. Prevalence, Patterns, and Associated Factors for Musculoskeletal Disorders Among the Healthcare Workers of Northern Saudi Arabia: A Multicenter Cross-Sectional Study. J Pain Res [Internet]. 2023;16:3735-46. doi: https://doi.org/10.2147/JPR.S415919
39. Alnaami I, Awadalla NJ, Alkhairy M, Alburidy S, Alqarni A, Algarni A, et al. Prevalence and factors associated with low back pain among health care workers in southwestern Saudi Arabia. BMC Musculoskelet Disord [Internet]. 2019;20(1):56. doi: https://doi.org/10.1186/s12891-019-2431-5
40. Meraz-Medina T, Zamora-Sánchez NF, Maldonado-Suárez N, Santoyo-Telles F. Depression, anxiety and stress levels among frontline healthcare workers during COVID-19 in Jalisco, Mexico. RIDE [Internet]. 2023;13(26). doi: https://doi.org/10.23913/ride.v13i26.1474
41. Jeleff M, Traugott M, Jirovsky-Platter E, Jordakieva G, Kutalek R. Occupational challenges of healthcare workers during the COVID-19 pandemic: a qualitative study. BMJ Open [Internet]. 2022;12:e054516. doi: https://doi.org/10.1136/bmjopen-2021-054516
42. Cohen C, Pignata S, Bezak E, Tie M, Childs J. Workplace interventions to improve well-being and reduce burnout for nurses, physicians and allied healthcare professionals: a systematic review. BMJ Open [Internet]. 2023;13(6):e071203. doi: https://doi.org/10.1136/bmjopen-2022-071203
43. Argus-Calvo B, Clegg DJ, Francis MD, Dwivedi AK, Carrola PA, Leiner M. A holistic approach to sustain and support lifelong practices of wellness among healthcare professionals: generating preliminary solid steps towards a culture of wellness. BMC Med Educ [Internet]. 2024;24(1):1364. doi: https://doi.org/10.1186/s12909-024-06353-7