Metric Properties of the Test of Infant Motor Performance in Colombian Children
Propiedades métricas del Test de Desarrollo Motor en niños colombianos
María Eugenia Serrano-Gómez, Martha Lucía Acosta-Otálora , Mónica Yamile Pinzón-Berna, Luisa Matilde Salamanca-Duque, Maritza Quijano Cuéllar, Jouvelly Catalina Malpica Río
Abstract
Objective. The objective of this research was to determine the metric properties of the Test of Infant Motor Performance (TIMP) adapted to Colombian Spanish.
Methods. This study evaluated a diagnostic test through analyses of metric properties, i.e., internal consistency, interrater reliability and concurrent validity. The unit of analysis was the Test of Infant Motor Performance. A sample of 112 children between 36 weeks postmenstrual age and 4 months of age was assessed. Two expert evaluators in the area of child neurorehabilitation, with expertise and training in the application of the instrument, participated. The internal consistency analysis was performed using Cronbach’s alpha coefficient. The interrater reliability evaluation was performed by calculating intraclass correlation coefficients. The Pearson correlation coefficient was used to determine concurrent validity. The analyses of the data obtained were performed using SPSS version 27.0.
Results. The Cronbach’s α was between 0.61 and 0.84. For the reliability, the instrument revealed an intraclass correlation coefficient between 0.54 and 0.93. The concurrent validity showed a Pearson correlation coefficient of 0.82.
Conclusions. The TIMP adapted to Colombian Spanish is a valid and reliable instrument that can be used for the assessment of motor performance in children.
Keywords
Test of Infant Motor Performance; psychometry; reproducibility of the results; validity of the results; motor skills; premature birth; physical therapy; interrater reliability; neurological risk.
Resumen
Objetivo. El objetivo de esta investigación fue determinar las propiedades métricas del Test de Rendimiento Motor Infantil (TIMP) adaptado al español de Colombia.
Métodos. Este estudio evaluó una prueba diagnóstica mediante análisis de propiedades métricas, es decir, consistencia interna, confiabilidad interevaluadores y validez concurrente. La unidad de análisis fue el Test de Rendimiento Motor Infantil. Se evaluó una muestra de 112 niños de entre 36 semanas de edad postmenstrual y 4 meses de edad. Participaron dos evaluadores expertos en el área de la neurorrehabilitación infantil, con experiencia y formación en la aplicación del instrumento. El análisis de consistencia interna se realizó mediante el coeficiente alfa de Cronbach. La evaluación de la fiabilidad entre evaluadores se realizó mediante el cálculo de los coeficientes de correlación intraclase. Para determinar la validez concurrente se utilizó el coeficiente de correlación de Pearson. Los análisis de los datos obtenidos se realizaron con el programa SPSS versión 27.0.
Resultados. El α de Cronbach se situó entre 0,61 y 0,84. En cuanto a la fiabilidad, el instrumento arrojó un coeficiente de correlación intraclase entre 0,54 y 0,93. La validez concurrente arrojó un coeficiente de correlación de Pearson de 0,82.
Conclusiones. El TIMP adaptado al español colombiano es un instrumento válido y confiable que puede ser utilizado para la evaluación del desempeño motor en niños.
Palabras clave
Test de Desarrollo Motor Infantil; psicometría; reproducibilidad de los resultados; validez de los resultados; habilidades motoras; nacimiento prematuro; fisioterapia; confiabilidad inter evaluadores; riesgo neurológico.
Introduction
Timely responses arise from the early diagnosis and implementation of professional judgment based on critical reasoning regarding the health condition of an individual. To achieve this, a methodical and rigorous process that incorporates personal and contextual elements is necessary. Among these, it is essential to recognize risk factors that may influence the development of health conditions.
The neonatal and postnatal stages are of great importance for development. The timely and pertinent response to possible complications or risk indicators can minimize sequelae and positively impact the quality of life of neonates and their family.
The World Health Organization (WHO) estimates that among newborns who are products of pregnancies classified as “high risk,” 3 to 5% are born at neurological risk. A newborn with high neurological risk is considered to have a history that can influence his or her development and favor outcomes related to cognitive, motor, sensory or behavioral limitations, which may be transitory or permanent [1].
There are several factors that are associated with neurological risk in neonates. Among these, low birth weight and premature birth play important roles and predispose neonates to the development of functional conditions with some type of limitation [2].
According to the Global Action Report on Premature Births, approximately 15 million children are born prematurely each year; approximately 7% of these children die, and many others suffer some type of physical or cognitive disability, resulting in high family and social costs [3]. In Colombia, premature births account for 9.07% of live births [4].
Regardless of gestational age, it is important to identify neurological risk early because the mechanisms of neuronal plasticity in the first months of life play fundamental roles in the creation of brain engrams conducive to the optimization of development and provision of neural resources for adaptation and functional reorganization [5].
For this, the early detection of neurological risk requires the use of valid and reliable measurement instruments, which allow guiding the diagnosis and implementation of interactive plans to prevent sequelae, functional limitations and disability and favor the integral development of the child and his or her quality of life [6].
The above is consistent with the support offered in the Guide for Physical Therapy Practice of the American Physical Therapy Association (APTA) regarding the importance of issuing a timely and accurate diagnosis, which leads to the establishment of early interventions and contributes to the neuromotor and sensorimotor development of the child [7].
There are several assessment instruments that measure neuromotor function in children during their first months of life, but it is important to use validated and reliable tools in the language of the context in which they are applied to ensure sound decisions regarding neuromotor function to facilitate development and improve prognosis.
As stated above, there is a sizable rate of premature births in Colombia, and the health programs for this population do not have standardized, valid, and reliable assessment tools to be used before the child reaches the corrected age of 40 weeks. This limits the possibility of an early intervention and the potential effect of neuroplasticity for the child’s neurodevelopment.
The above was considered as a decision criterion to guide the choice of the Test of Infant Motor Performance (TIMP; Prueba de Rendimiento Motor Infantil -PRMI- in Spanish) as the instrument to be studied in this research. In addition to evaluating neuromotor function after the age equivalent to term (40 weeks postconception), the TIMP is one of the few tools that allows assessing this category in premature children from week 34 postconception and has proven to be a tool with high sensitivity and specificity and high predictive power about neurological risk [8,9].
It is worth noting that the TIMP is listed as a pediatric assessment tool in the International Classification of Functioning, Disability and Health (ICF) and by the pediatric section of the APTA [10].
A version of the TIMP is available in Colombia; this version was translated, cross-culturally adapted and validated, with metric properties similar to those for the original version. The adjustments to Colombian Spanish were applied mainly from a semantic perspective. The back-translation stage and the validation did not show significant discursive problems. With this, the translation and cross-cultural adaptation was considered successful from the perspectives of validity and appearance for the Colombia context [11].
The objective of this research was to determine the internal consistency, interrater reliability and concurrent validity of the Test of Infant Motor Performance adapted to Colombian Spanish when used to assess children up to 4 months of age.
Methods
This is an instrumental study [12]. The TIMP -version adapted to Colombian Spanish (PRMI)- was assessed through analyses of metric properties for its internal consistency, interrater reliability, and concurrent validity.
The PRMI version for Colombia, developed from the official versions in English and in Spanish (Spain), is a valid, reliable, and culturally appropriate tool [11].
To calculate the sample size, the recommendation by Kline [13] was taken into account, i.e. the number of subjects aimed to be at least double or triple the number of variables in the measurement instrument. The present investigation then decided to consider a number of subjects that represented three times the variables contained in the test. Considering that the TIMP contains 42 variables but 6 of these are the same variable applied to each of the hemibodies, 36 variables were examined for the calculation of the sample size, along with a 4% estimated dropout rate. For this reason, the metric properties of the TIMP were analyzed based on a sample of 112 children, between 36 weeks postmenstrual age and 4 months of age from the cities of Bogotá and Manizales in Colombia. These children were assessed at the Hospital de La Samaritana (an axis for a network of 37 hospitals in the department of Cundinamarca and a point of reference in health, offering coverage within 116 municipalities in Colombia) and at the Corporación Sagrada Familia, a Non-Governmental Organization. The assessment was conducted between February and August 2021 using a single video recording per participant.
The participants were selected deliberately, considering their total meeting of the following inclusion criteria: children up to 4 months of age, children born prematurely and at term, female or male, hemodynamically stable and discharged from the health institution, and children whose parents or legal guardians authorized their participation in the study.
The exclusion criteria were children with health conditions that made assessment difficult (e.g., fever, pain, and sepsis) and children with chromosomal syndromes.
Variables
The study variables included sex, type of birth by gestational age, corrected age for premature children and chronological age for term children, health conditions, the city of assessment and the area of origin (urban or rural). The main variables of the study were the observed and elicited items of the PRMI and of the Alberta Infant Motor Scale.
Evaluators
Two evaluators with expertise in the area of child neurorehabilitation, who performed a prior training process through the TIMP online platform (http://www.thetimp.com/products-for-therapists#!/The-TIMP-Online-Individuals/p/56137131/category=100056112), participated.
Additionally, 5 observation sessions of children under 4 months of age were carried out to acquire skills in the use of the instrument and to standardize the test criteria.
Instruments
Sociodemographic questionnaire
A questionnaire for sociodemographic variables was conducted through an interview with the mother or legal guardian of the child, through which some clinical and demographic characteristics of the child and their family were identified.
The instrument used to gather data was the product of the translation and cross-cultural adaptation of the TIMP into Colombia Spanish (PRMI in Spanish). In addition, the Alberta Infant Motor Scale (AIMS) was used as a reference test to determine the concurrent validity of the PRMI.
Test of Infant Motor Performance
The TIMP was designed by Suzann Campbell, Gay Girolami, Thugi Kolobe, Elisabeth Osten, and Maureen Lenke in 1995. The instrument, which was originally in English, has been officially translated into Portuguese, French, and Spanish and allows the evaluation of the motor performance of children born at term and premature from week 34 postmenstrual until 4 months of age. The TIMP has 42 items grouped up in two sections: 13 observed items concerning spontaneous activities in the infant and evaluated through observation without manipulation, and 29 provoked items that must be induced through provocation maneuvers. The test evaluates the motor performance of children, including postural control and selective motor control through the observation and provocation of movement patterns essential for the development of functional activities. The TIMP has been shown to discriminate the severity of motor impairment, to diagnose delays in motor development, to predict motor performance, and to measure the effects of interventions and has been used to educate parents about their child’s motor development and to research motor development in clinical trials [8,14]. It is a noninvasive clinical evaluation instrument with minimal requirements and adequate metric properties that ensures consistent and significant results in relation to the motor repertoire of children who exhibit neuromotor alterations and a greater risk of long-term disability [15-17].
The items of the TIMP are grouped into 7 categories: 1) spontaneous activity/observed items (Items 1-13); 2) alignment-head control (Items 14-18); 3) head and trunk control in the supine position (Items 19-27); 4) rolling (Items 28-31); 5) antigravity control of the head, trunk and hip (Items 32-34); 6) head and trunk control in the prone position (Items 35-39); and 7) lateral control of the head and standing (Items 40-42). The above, obtained from TIMP Online, were devised by Suzann Campbell [8].
The total score is obtained by summing the scores for all items contained in the 2 sections (ranging from 0 to 142 points) and is interpreted using a table of percentiles. The delay threshold corresponds to the 25th percentile. When a child is in an environment that allows the adequate demonstration of his or her motor repertoire, the application time varies between 20 and 45 minutes [8].
In general, the TIMP is considered an instrument par excellence for the evaluation of motor performance and the determination of the need for intervention at an early age in at-risk infants [17].
The TIMP has traditionally been shown to have adequate metric properties for its application in children up to 4 months of age [11,14-22]. It is sensitive to changes in the development of functional motor skills depending on age and to the risk of low performance results or motor performance [23]. In addition to its adequate validity and reliability properties, it has important predictive value. It has been shown, for example, that TIMP scores at 12 weeks of corrected age predict motor outcomes at 1 year and 5 years of age [24].
A prospective study conducted with high-risk premature infants found that the scores obtained through this instrument, applied at 10 to 15 weeks of corrected age, were significantly related not only to motor results but also to cognitive and language outcomes at 2 years of corrected age [14]. The results show that the TIMP is a relevant instrument for predicting outcomes related to motor performance [25] and to other areas of development, such as cognition and communication. Children who exhibit poorer motor performance in the TIMP at 3 months of age may be more likely to have adverse neurodevelopmental outcomes at 2 years of age or older [14].
Alberta Infant Motor Scale (AIMS)
This scale was developed by Martha Piper and Johanna Darrah in 1994 and is designed to evaluate the gross motor development of children (born at term and premature) from full-term to 18 months. The AIMS is applied in the prone, supine, sitting and bipedal positions and contains a total of 58 items that must be evaluated considering 3 attributes: posture, weight transfer, and antigravity movement. Its application is carried out through the observation of the motor repertoire demonstrated by the child, the results of which determine the “motor window of the infant.” The results are interpreted using a table of percentiles, and the application time varies between 15 and 20 minutes when the evaluator is experienced and the disposition of the child readily allows the assessment [26-33].
Ethical Considerations
The current study was approved by the Committee of Ethics in Research of the Universidad de La Sabana, Act # 65 of 2018 and registry code number ENF-23-2017; by the Bioethics Committee of the Universidad Autónoma de Manizales, Act # 088 of 2019 and by the Committee of Ethics in Research of the La Samaritana University Hospital, Act # 02-2020. All of the infants' parents were made aware of the project's objective and procedures; they all signed the informed consent form voluntarily after reading it and having it explained to them. This research considered the international guidelines for ethics in scientific writing, as well as those to maintain the integrity and confidentiality of all participants for the study, in consideration of the privacy and autonomy principles established by the Declaration of Helsinki and the guidelines of Resolution 8430 of 1993 by the Health Ministry of Colombia [34,35].
Procedure
Between the months of February and August 2021, the researchers assessed the children using a single video recording per participant. The duration of each assessment ranged from 20 to 45 minutes. During the first minutes, each child was assessed through the AIMS, which took a short time given the motor repertoire for their age range. Afterwards, an evaluator applied the PRMI on a gurney in a warm and quiet space, with the child wearing only diapers and a tank top while awake and calm (Brazelton state 4); the other evaluator recorded the necessary video. Items used for the test included a small red ball, a squishy and squeaky toy, a baby rattle, and a soft cloth following the standardized guidelines for the test. The preterm infants were evaluated according to their corrected age while chronological age was used for term infants.
To analyze interrater reliability and internal consistency, the evaluators observed each video and completed the PRMI independently. To analyze concurrent validity, the evaluators also completed the AIMS, considered a reference test for the motor evaluation of children during their first year and a half of postnatal life [24,28-33].
Analysis
Reliability was assessed through internal consistency and interrater reliability. Internal consistency was determined using Cronbach's alpha coefficient (α). Interrater reliability was assessed by calculating the Intraclass Correlation Coefficient that allows the measurement of the agreement between 2 or more quantitative assessments obtained from different raters. Values between 0.41 and 0.60 indicate that the reliability or agreement between the measurements is moderate; values between 0.61 and 0.8 indicate that the reliability or agreement is substantial; and values between 0.81 and 0.99 indicate that the reliability or agreement is almost perfect [36].
Concurrent validity was assessed by calculating the Pearson correlation coefficient, which ranges from -1 to 1; the closer the results are -in relative terms- the greater the degree of validity. To obtain the results of the assessments of the children, their raw scores were used as the measurement; therefore, the analysis was done considering a ratio scale for the PRMI and the AIMS [37].
Results
To interpret the results, the items of the PRMI were grouped into 7 categories: 1) spontaneous activity/observed items; 2) alignment-head control; 3) head and trunk control in the supine position; 4) rolling; 5) antigravity control of the head, trunk and hip; 6) head and trunk control in the prone position; and 7) lateral control of the head and standing.
Sociodemographic and clinical characteristics of the sample
This study included 112 children assessed at the Hospital de La Samaritana and at the Corporación Sagrada Familia in Bogota and Manizales, Colombia. Mean age was 2.08 months with a minimum -4 weeks (36 weeks postmenstrual age) and a maximum 17 weeks
In terms of sex and city of assessment, the sample was uniform, with low selection bias. Regarding area of origin, most of the children came from the urban areas; the majority of the mothers had complete secondary schooling and reported a middle socioeconomic status (Table 1).
Table 1. Sociodemographic variables of the study participants.
| Sociodemographic variables | Sample (n = 112) | ||
|---|---|---|---|
| Absolute frequency | Relative frequency (%) | ||
| Sex | Male | 57 | 50.9 |
| Female | 55 | 49.1 | |
| City of assessment | Manizales | 55 | 49.1 |
| Bogotá | 57 | 50.9 | |
| Area of origin | Rural | 20 | 17.9 |
| Urban | 92 | 82.1 | |
| Socioeconomic status | Low | 52 | 46.4 |
| Middle | 60 | 53.6 | |
| Mother's education level | Complete elementary schooling | 23 | 20.5 |
| Complete secondary schooling | 74 | 66.1 | |
| Higher education | 15 | 13.4 | |
Note. Source: Own elaboration.
Clinical variables
Clinical variables such as type of birth by gestational age and health conditions were registered. Regarding gestational age, most of the children were born at term. Regarding health conditions, 5.4% of the children were diagnosed with low birth weight, and 13.4% were diagnosed with other medical diagnoses, such as bleeding sequelae, cerebral hypoxia, neonatal infection, intrauterine growth restriction, endocrine and metabolic disorders, congenital syphilis, toxoplasmosis, agenesis of the auricle, horseshoe kidney, congenital clubfoot, and persistent foramen ovale (Table 2).
Table 2. Clinical variables.
| Clinical variables | Sample (n = 112) | ||
|---|---|---|---|
| Absolute frequency | Relative frequency (%) | ||
| Type of birth by gestational age | Full-term birth | 68 | 60.7 |
| Premature birth | 44 | 39.3 | |
| Health conditions | Without medical diagnosis | 47 | 41.9 |
| Prematurity | 44 | 39.3 | |
| Low birth weight | 6 | 5.4 | |
| Other diagnoses | 15 | 13.4 | |
Note. Source: Own elaboration.
Internal consistency
For all categories, Cronbach’s α was between 0.61 and 0.84, demonstrating an internal consistency that ranged from substantial to almost perfect (Table 3).
Table 3. Results for the internal consistency of the PRMI.
| DIMENSION | α CRONBACH |
|---|---|
| Category 1 | 0.70 |
| Category 2 | 0.84 |
| Category 3 | 0.61 |
| Category 4 | 0.73 |
| Category 5 | 0.70 |
| Category 6 | 0.77 |
| Category 7 | 0.80 |
Note. Source: Own elaboration.
Interrater reliability
The intraclass correlation coefficients for the categories in which the items of the PRMI are grouped were as follows: Category 1, 0.54 (moderate agreement); Category 2, 0.88 (almost perfect agreement); Category 3, 0.8 (substantial agreement); Category 4, 0.9 (almost perfect agreement); Category 5, 0.81 (almost perfect agreement); Category 6, 0.93 (almost perfect agreement) and Category 7, 0.69 (substantial agreement). Overall, the IIC for the provoked items (Categories 2-7) was 0.93, representing almost perfect agreement between the evaluators (Table 4).
Table 4. Results for the interrater reliability of the PRMI.
| Dimension | Intraclass Correlation Coefficient | Type of Agreement | IC (95%) | P Value |
|---|---|---|---|---|
| Category 1. Total Observed Items | 0.54 | Moderate | (0.33-0.68) | 0.000 |
| Category 2 | 0.88 | Almost perfect | (0.82-0.92) | 0.000 |
| Category 3 | 0.8 | Substantial | (0.7-0.86) | 0.000 |
| Category 4 | 0.9 | Almost perfect | (0.86-0.93) | 0.000 |
| Category 5 | 0.81 | Almost perfect | (0.73-0.87) | 0.000 |
| Category 6 | 0.93 | Almost perfect | (0.9-0.95) | 0.000 |
| Category 7 | 0.69 | Substantial | (0.55-0.79) | 0.000 |
| Total Provoked Items | 0.93 | Almost perfect | (0.9-0.95) | 0.000 |
Note. Source: Own elaboration.
Concurrent validity
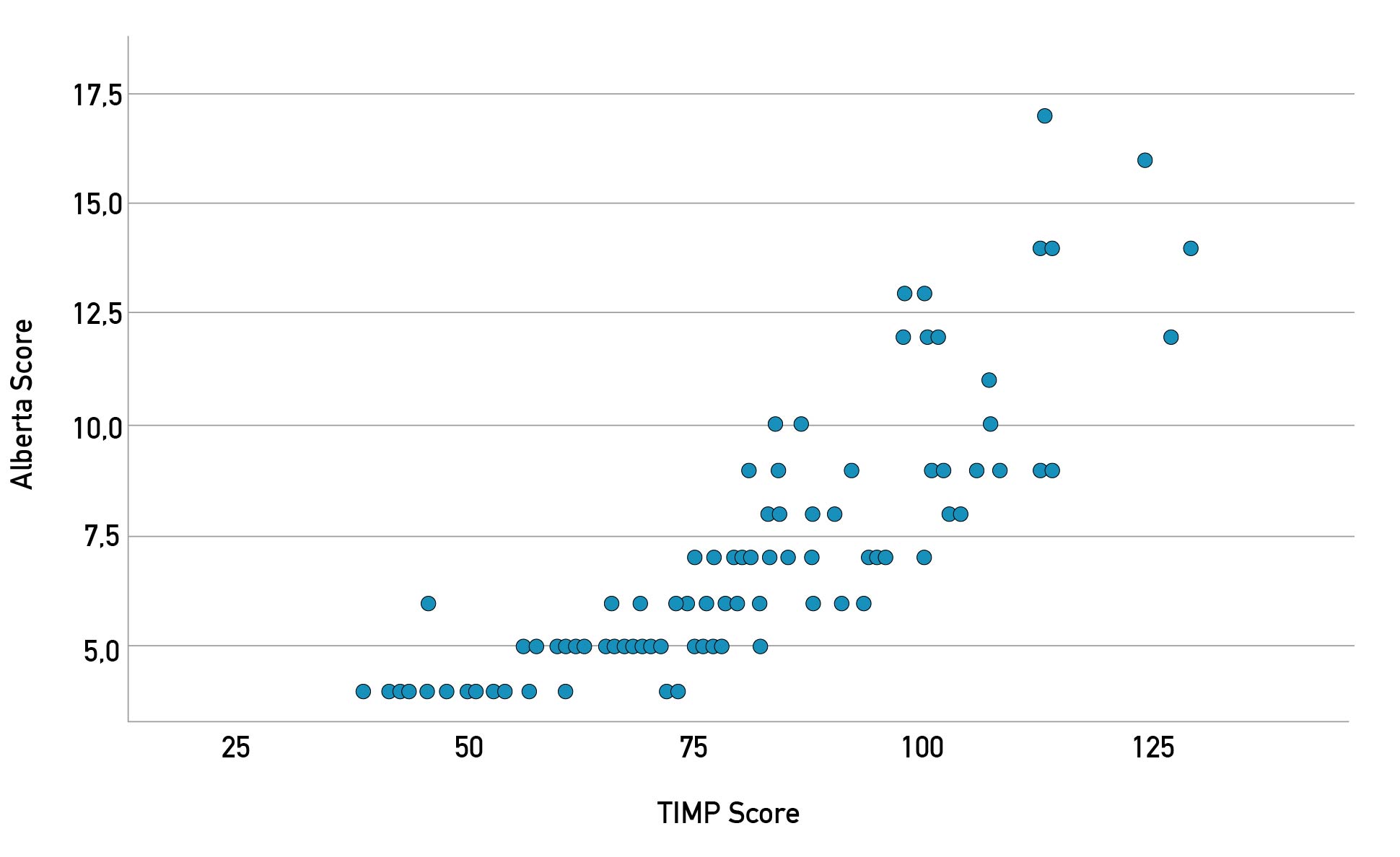
The Pearson Correlation Coefficient for concurrent validity was 0.82 (p < 0.001), indicating a highly positive correlation between the PRMI and AIMS (Figure 1).
Figure 1. Concurrent validity results for the PRMI.
Discussion
Early and timely diagnoses require valid and reliable instruments to detect neuromotor risk and predict the development of children in the short and medium terms. To ensure accuracy, it is important for instruments to have translated and cross-culturally adapted versions. Therefore, the objective of this research was to determine the internal consistency, interrater reliability, and concurrent validity of the Test of Infant Motor Performance adapted to Colombian Spanish (PRMI) when used to assess children up to 4 months of age.
The results of this study showed that the PRMI has an internal consistency between substantial and almost perfect (Cronbach’s α of 0.70 for the observed items and between 0.61 and 0.84 for the provoked items). A similar finding was reported by a study conducted with children in Brazil when applying the Portuguese version of the TIMP; the internal consistency was between substantial and almost perfect (Cronbach’s α of 0.71 for the observed items and 0.98 for the provoked items) [16]. For the Spanish version, Echevarría reported an internal consistency greater than 0.95, a value that, likewise, confirms an almost perfect degree of correlation between the items [9]. According to the study conducted in Nepal, Alphas for the TIMP total scores were 0.72 for infants born preterm and 0.76 in those born to term [17]. Additionally, the TIMP´s Persian version exhibited a high internal consistency (α = 0.82) when applied to Persian children [38].
Regarding the reliability of the PRMI, the results of this study showed high levels of agreement between the raters (interrater reliability): within the moderate range for the observed items and almost perfect range for the provoked items. Similarly, the reliability results for a Brazilian study conducted with local children indicated a high level of agreement between the evaluators: the ICCs were between 0.65 and 0.99, with the lowest scores being those obtained for the observed items (ICCs between 0.65 and 0.83) [16]. These similarities remained in yet another study conducted in Nepal with local children, with ICCs >0.93 [17]. Its metric properties have also been evaluated in Persian children with high results for its intra and inter-rater reliability (ICC = 0.98, Kappa = 0.93) and test-retest reliability (ICC = 0.98) [38].
Likewise, other studies have found that the TIMP is a reproducible instrument, with varying ICC values, i.e., 0.79 [39], 0.95 [40] and 0.99 [18].
In addition to the above, a study of the reliability of the TIMP showed that the tests can be administered safely and effectively in children with hypotonia and weakness, such as type I spinal muscular atrophy; the results indicated that the interrater reliability had an overall weighted Kappa of 0.61 (95% CI: 0.59-0.63) [41].
Regarding concurrent validity, the results of this study showed that the PRMI and AIMS are positively correlated (Pearson Correlation Coefficient of 0.82). This value was higher than those obtained by Campbell & Kolobe, who reported correlation coefficients of 0.64 between the scores of the 2 instruments and of 0.60 between the TIMP scores and the percentile ranges of the AIMS; likewise, the agreement corrected by chance (Kappa Coefficient) between the 2 instruments was 0.41 [21]. In addition to this, there´s evidence that supports the content validity and face validity of the TIMP having been confirmed by an expert’s panel and 10 therapists in Persia [38].
The TIMP is a standardized test that requires expertise from the examiner and precise handling so that its administration does not suppose a bias, altering the results of the test. Due to this, the level of agreement between examiners in the present study reflects the relevance of previous training for evaluators; the recommendations contained in both the user manual and the TIMP Online developed by Suzann Campbell provide valuable information to apply the instrument and obtain reproducible measurements. Likewise, the results from this study illustrate how the protocol designed for data collection was adequate, as it allowed the conception of a process aiming towards the proper administration of the test from the evaluators, which reduced the risk of examiner bias.
In this study, the internal consistency of the observed items of PRMI was lower than the internal consistency for other categories, similar to how the study carried out in Brazil reported it [16]. This may be due to the fact that the items from this category are more variable than for the other categories in terms of their nature and presentation; it includes spontaneous movements, general movements with predictive capacity, items that show the ability of the child to center his posture and body parts around his midline, and activities from the repertoire of primary movements of functional ability and antigravitational activities. Something similar could have been the cause of the results for categories 3 and 5, which demonstrated lower internal consistency than the other categories.
Furthermore, the inter-rater reliability, which was moderate for the observed items and between substantial and almost perfect for the obtained items, could then be positively related to the prior training that the raters received. This was done individually through TIMP Online and through group discussions and consensus based on resources such as the TIMP manual, videos for evaluator calibration, and documents related to the theoretical and research bases of the instrument, among other resources. The differences found between evaluators could depend on the experience of the evaluator and the environment and context in which the TIMP was applied and interpreted, additionally in some cases, the child's performance could be underestimated or overestimated. Moreover, it is important to note that the scoring of the items in this instrument is based primarily on qualitative observations, so there is greater potential for differences between raters, particularly for the 13 observed items that require greater attention and skill to analyze and evaluate because they are items whose possibility of response is dichotomous (present-absent) and depends on the child's spontaneous reactions.
Notably, the use of tools such as the PMRI allows a standardized and rigorous assessment and provides a guide to the early diagnosis of children with suspected neurological risk; this facilitates the establishment of timely intervention strategies that can significantly impact functional prognoses.
This study found limitations due to the health emergency of the Covid-19 pandemic, because of which the data recollection planned to be carried out during 2020 had to be postponed. Likewise, during the time in 2021 when it was possible to collect data, the evaluators still found significant restrictions to access the assessment of the children participating in the study.
In addition, although the assessments were all completed, there is an acknowledgement of the fact that some of the children were irritable, agitated, intolerant, and defensive in certain positions to generate optimal responses and easily observable performances for the respective items. This meant a variability in the scores given by the evaluators.
As a strength for the study, it is remarked that no adverse effects were found as a result of the usage of the tool.
Although there are important advances in research on the early detection of neurological risk, it is important to continue strengthening strategies to minimize the impact that functional limitations or disability may generate, secondary to erroneous or late diagnoses.
Conclusions
The results obtained suggest that the version of the TIMP adapted to Colombian Spanish is a valid and reliable instrument that requires expertise and training and can be used for the assessment of motor performance in children; it is a useful and recommended tool to guide diagnoses related to the motor function of children up to 4 months of age.
The findings of this study indicate that the PRMI has adequate interrater validity and reliability properties for its application in Colombia; hence, it has clinical utility with regard to the identification of children with long-term neurological risk.
Nevertheless, new studies with wider and diverse population samples -in which new psychometric properties can be defined for their application in Colombian populations- are required.
References
1. Ramos I, Márquez A. Recién nacido de riesgo neurológico. Vox Paediatrica [Internet]. 2000;8(2):5-10. Available from: https://spaoyex.es/voxp/volumen-8-2000-n-2
2. Rodríguez-Valdés R, Aguilar-Fabré L, Rivera-Alés L, Galán-García L, Aguilar-Fabré K, Barrera-Sánchez J, et al. Estudio clínico y electroencefalográfico en lactantes con factores de riesgo de daño neurológico. Rev mexicana de neurociencia [Internet]. 2018;19(4):25-35. doi: https://doi.org/10.31190/rmn.2018.19.4.25.35
3. World Health Organization (WHO) [Internet]. Geneva: WHO; c2024. Nacimientos Prematuros; 2018 Feb 19 [updated 2023 May 11; cited Jan 16 2023]; [about 4 screens]. Available from: https://www.who.int/es/news-room/fact-sheets/detail/preterm-birth
4. Ospino M, Mercado M. Comportamiento de la Prematuridad en Colombia Durante los Años 2007 a 2016. Poster session presented at: XII International Conference on KMC; 2018 Nov 14-17; Bogotá, Colombia. Available from: https://fundacioncanguro.co/documentacion-canguro/#XII_Encuentro_Internacional_sobre_el_MMC_%E2%80%93_Bogot%C3%A1_Colombia_2018_
5. Ismail FY, Fatemi A, Johnston MV. Cerebral plasticity: Windows of opportunity in the developing brain. Eur J Paediatr Neuro [Internet]. 2017;21(1):23-48. doi: https://doi.org/10.1016/j.ejpn.2016.07.007
6. Hadders-Algra M. Early Diagnostics and Early Intervention in Neurodevelopmental Disorders-Age-Dependent Challenges and Opportunities. J Clin Med [Internet]. 2021;10(4):1-23. doi: https://doi.org/10.3390/jcm10040861
7. American Physical Therapy Association. Guide to Physical Therapist Practice. 3rd Edition. Alexandria: American Physical Therapy Association APTA. 2014. 22-23 p.
8. Campbell S. The Test of infant motor performance: Test user’s manual version 3.0 for the TIMP version 5. Chicago: Infant Motor Performance Scales, LLC; 2012. 65 p.
9. Echevarría Ulloa M. Adaptación transcultural y versión española de la prueba de rendimiento motor infantil (TIMP) [doctoral dissertation]. Madrid: Universidad Complutense de Madrid; 2017. 121 p. Available from: https://hdl.handle.net/20.500.14352/22237
10. Academy of Pediatric Physical Therapy (APTA). Fact Sheet. List of Pediatric Assessment Tools Categorized by ICF Model [Internet]. 2013. 6 p. Available from: https://pediatricapta.org/includes/fact-sheets/pdfs/FactSheet_ListofPediatricAssessmentToolsCategorizedbyICFModel_2013.pdf
11. Naranjo Ruiz M, Guerrero Uchima IG, Serrano Gómez ME, Acosta Otálora ML, Pinzón Bernal MY, Salamanca Duque LM. Translation and Cross-Cultural Adaptation of the Test of Infant Motor Performance to Colombian Spanish. Rev Cienc Salud [Internet]. 2022;20(1):1-17. doi: https://doi.org/10.12804/revistas.urosario.edu.co/revsalud/a.10146
12. Carretero-Dios H, Pérez C. Standards for the development and review of instrumental studies: Considerations about test selection in psychological research. In J Clin Health Psychol [Internet]. 2007;7(3):863-82. Available from: https://www.redalyc.org/articulo.oa?id=33770319
13. Kline P. An Easy Guide to Factor Analysis [Internet]. London: Routledge; 2014. 208 p. doi: https://doi.org/10.4324/9781315788135
14. Peyton C, Schreiber MD, Msall ME. The Test of Infant Motor Performance at 3 months predicts language, cognitive, and motor outcomes in infants born preterm at 2 years of age. Dev Med Child Neurol [Internet]. 2018;60(12):1239-43. doi: https://doi.org/10.1111/dmcn.13736
15. Kim SA, Lee YJ, Lee YG. Predictive Value of Test of Infant Motor Performance for Infants based on Correlation between TIMP and Bayley Scales of Infant Development. Ann Rehabil Med. [Internet]. 2011;35(6):860-6. doi: https://doi.org/10.5535/arm.2011.35.6.860
16. Chiquetti EMS, Valentini NC, Saccani R. Validation and Reliability of the Test of Infant Motor Performance for Brazilian Infants. Phys Occup Ther Pediatr. [Internet]. 2020;40(4):470-85. doi: https://doi.org/10.1080/01942638.2020.1711843
17. Kvestad I, Silpakar JS, Hysing M, Ranjitkar S, Strand TA, Schwinger C, et al. The reliability and predictive ability of the Test of Infant Motor Performance (TIMP) in a community-based study in Bhaktapur, Nepal. Infant Behav Dev [Internet]. 2023;70:101809. doi: https://doi.org/10.1016/j.infbeh.2023.101809
18. Ustad T, Helbostad JL, Campbell SK, Girolami GL, Jørgensen L, Øberg GK, et al. Test-retest reliability of the Test of Infant Motor Performance Screening Items in infants at risk for impaired functional motor performance. Early Hum Dev. [Internet]. 2016;93:43-6. doi: https://doi.org/10.1016/j.earlhumdev.2015.12.007
19. Noble Y, Boyd R. Neonatal assessments for the preterm infant up to 4 months corrected age: A systematic review. Dev Med Child Neurol. [Internet]. 2012;54(2):129-39. doi: https://doi.org/10.1111/j.1469-8749.2010.03903.x
20. Spittle AJ, Doyle LW, Boyd RN. A systematic review of the clinimetric properties of neuromotor assessments for preterm infants during the first year of life. Dev Med Child Neurol. [Internet]. 2008;50(4):254-66. doi: https://doi.org/10.1111/j.1469-8749.2008.02025.x
21. Campbell S, Kolobe T. Concurrent validity of the test of infant motor performance with the Alberta Infant Motor Scale. Pediatr Phys Ther. [Internet]. 2000;12(1):2-9. Available from: https://journals.lww.com/pedpt/abstract/2000/01210/concurrent_validity_of_the_test_of_infant_motor.2.aspx
22. Echevarria M, Arroyo O, Lavin JL, Ubeda A, Martin P, Sanchez M. Spanish version of the test of infant motor performance (TIMP): Initial phase of cultural adaptation. J Perinat Med. [Internet]. 2015;43. Available from: https://www.degruyter.com/document/doi/10.1515/jpm-2015-2003/html
23. Campbell S, Kolobe T, Osten E, Lenke M, Girolami G. Construct validity of the test of infant motor performance. Phys Ther [Internet]. 1995;75(7):585-96. doi: https://doi.org/10.1093/ptj/75.7.585
24. Campbell S, Kolobe T, Wright B, Linacre J. Validity of the Test of Infant Motor Performance for prediction of 6-, 9- and 12-month scores on the Alberta Infant Motor Scale. Dev Med Child Neurol [Internet]. 2002;44(4):263-72. doi: https://doi.org/10.1111/j.1469-8749.2002.tb00802.x
25. Rose RU, Westcott SL. Responsiveness of the Test of Infant Motor Performance (TIMP) in infants born preterm. Pediatr Phys Ther [Internet]. 2005;17(3):219-24. doi: https://doi.org/10.1097/01.PEP.0000176575.63915.67
26. Piper M, Darrah J. Motor Assessment of the Developing Infant. Alberta Infant Motor Scale (AIMS). 2nd ed. Ámsterdam: Elsevier; 2021. 288 p.
27. Serrano ME, Camargo DM. Reproducibilidad de la Escala Motriz del Infante de Alberta (Alberta Infant Motor Scale) aplicada por fisioterapeutas en formación. Fisioterapia [Internet]. 2013;35(3):112-8. doi: https://doi.org/10.1016/j.ft.2012.09.002
28. Morales-Monforte E, Bagur-Calafat C, Suc-Lerin N, Fornaguera-Marti M, Cazorla-Sanchez E, Girabent-Farres M. The Spanish version of the Alberta Infant Motor Scale: Validity and reliability analysis. Dev Neurorehabil [Internet]. 2017;20(2):76-82. doi: https://doi.org/10.3109/17518423.2015.1066461
29. Syrengelas D, Siahanidou T, Kourlaba G, Kleisiouni P, Bakoula C, Chrousos GP. Standardization of the Alberta infant motor scale in full-term Greek infants: Preliminary results. Early Hum Dev [Internet]. 2010;86(4):245-9. doi: https://doi.org/10.1016/j.earlhumdev.2010.03.009
30. de Albuquerque PL, de Farias Guerra MQ, de Carvalho Lima M, Eickmann SH. Concurrent validity of the Alberta Infant Motor Scale to detect delayed gross motor development in preterm infants: A comparative study with the Bayley III. Dev Neurorehabil [Internet]. 2018;21(6):408-14. doi: https://doi.org/10.1080/17518423.2017.1323974
31. Pin TW, de Valle K, Eldridge B, Galea MP. Clinimetric properties of the Alberta Infant Motor Scale in infants born preterm. Pediatr Phys Ther [Internet]. 2010;22(3):278-86. doi: https://doi.org/10.1097/PEP.0b013e3181e94481
32. Uesugi M, Tokuhisa K, Shimada T. The reliability and validity of the Alberta Infant Motor Scale in Japan. Journal of physical therapy science [Internet]. 2008;20(3):169-75. doi: https://doi.org/10.1589/jpts.20.169
33. Rau MP, Hsue BJ, Ko YC, Lin YC. The concurrent validity of assessment of general movements with Alberta Infants Motor Scale. Physiotherapy [Internet]. 2015;101(Suppl 1):e1264. doi: https://doi.org/10.1016/j.physio.2015.03.1171
34. World Medical Association (WMA) [Internet]. Ferney-Voltaire: WMA; c2024. WMA declaration of Helsinki - Ethical principles for medical research involving human subjects; 2022 Sep 6 [updated 2023 May 11; cited Jan 16 2023]; [about 8 screens]. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/
35. Ministerio de Salud. Resolución No. 8430 de 1993, por la cual se establecen las normas científicas, técnicas y administrativas para la investigación en salud (Oct 4, 1993). Available from: https://www.minsalud.gov.co/salud/Lists/Normatividad%20%20Salud/DispForm.aspx?ID=2110&ContentTypeId=0x0100A08A4A1DF8E9D448BEF600BFAC0E7622
36. Castillo C, Corssen C, Breinbauer H, Namoncura C. Evaluación adenoídea mediante nasofaringolaringoscopía: validación del método. Rev Otorrinolaringol Cir Cabeza Cuello [Internet]. 2008;68(2):143-8. doi: https://doi.org/10.4067/S0718-48162008000200005
37. Schober P, Boer C, Schwarte LA. Correlation coefficients: Appropriate use and interpretation. Anesth Analg [Internet]. 2018;126(5):1763-8. doi: https://doi.org/10.1213/ANE.0000000000002864
38. Ravarian A, Rahmani N, Soleimani F, Sajedi F, Noroozi M, Campbell SK, et al. Test of infant motor performance: Cross-cultural adaptation, validity and reliability in Persian infants. Early Hum Dev [Internet]. 2023;184:105831. doi: https://doi.org/10.1016/j.earlhumdev.2023.105831
39. Campbell S, Zawacki L, Rankin K, Yoder J, Shapiro N, Li Z, et al. Concurrent validity of the TIMP and the Bayley III scales at 6 weeks corrected age. Pediatr Phys Ther [Internet]. 2013;25(4):395-401. doi: https://doi.org/10.1097/PEP.0b013e31829db85b
40. Lekskulchai R, Cole J. Effect of a developmental program on motor performance in infants born preterm. Aust J Physiother [Internet]. 2001;47(3):169-76. doi: https://doi.org/10.1016/S0004-9514(14)60264-6
41. Finkel R, Hynan L, Glanzman A, Owens H, Nelson L, Cone S, et al. The test of infant motor performance: Reliability in Spinal Muscular Atrophy Type I. Pediatr Phys Ther [Internet]. 2008;20(3):242-6. doi: https://doi.org/10.1097/PEP.0b013e318181ae96